
Risk-Benefit Calculator
How to Use This Tool
This calculator helps you understand the difference between relative and absolute risk, which is crucial for interpreting FDA drug labels. Enter a baseline risk and relative risk reduction percentage to see what this means in real terms.
Your Results
Enter your values above to see the calculation.
When you pick up a new prescription, the label that comes with it isn’t just a list of side effects. It’s a carefully written summary of whether the drug’s benefits are worth the risks - and for most patients, it’s nearly impossible to understand.
What Exactly Is a Risk-Benefit Statement?
The U.S. Food and Drug Administration (FDA) requires every prescription drug label to include a clear statement explaining why the benefits of the medicine outweigh its risks. This isn’t marketing fluff. It’s a formal, science-backed evaluation used to decide whether a drug gets approved at all. But what you see on the label is often a condensed version of a much deeper analysis done by FDA scientists.
For example, a cancer drug might show that it extends life by an average of 4 months but causes severe nausea in 60% of patients. The FDA weighs that trade-off: Is 4 more months of life worth enduring daily vomiting and fatigue? For someone with advanced cancer and no other options, the answer may be yes. For someone with early-stage disease and other treatments available, the answer might be no. The label doesn’t always make that distinction clear.
Where to Find the Risk-Benefit Info in the Label
You won’t find a single box labeled “Benefits vs. Risks.” Instead, the information is spread across several sections:
- Section 5: Contraindications - Lists when the drug should not be used, like in people with certain heart conditions or allergies.
- Section 6: Adverse Reactions - Details side effects, from mild (headache, dizziness) to serious (liver damage, heart rhythm issues).
- Section 8: Use in Specific Populations - Explains how the drug affects pregnant women, older adults, or people with kidney disease.
- Section 14: Clinical Studies - The most important part. This is where the FDA summarizes the actual data from trials: how many people improved, how many had bad reactions, and how the drug compared to a placebo or another treatment.
The Highlights section at the top gives a quick snapshot, but the real answers are buried in Section 14. That’s where you’ll see numbers like: “In a trial of 1,200 adults, 42% of those taking the drug saw their symptoms improve compared to 21% on placebo.” That’s a real benefit. Now look for the risk: “15% experienced serious liver injury.” That’s a real risk.
Why Most Patients Don’t Understand the Label
A 2022 survey of 1,842 patients found that only 22% felt confident they could interpret the risk-benefit info on their drug labels. Among those with low health literacy, that number dropped to 9%. Why? Because labels are written for regulators - not people.
Take a common phrase: “The relative risk of stroke was reduced by 30%.” Sounds good, right? But if your baseline risk of stroke is 2% per year, a 30% reduction means it drops to 1.4%. That’s a 0.6% absolute benefit - far less dramatic than it sounds. Patients often mistake relative risk for absolute risk, leading to false expectations.
Another problem: labels rarely compare the drug to alternatives. If you’re told a new diabetes drug reduces heart attack risk by 25%, you don’t know if that’s better or worse than metformin or insulin. The FDA doesn’t require that comparison, even though patients need it to make real decisions.
What’s Being Done to Fix This?
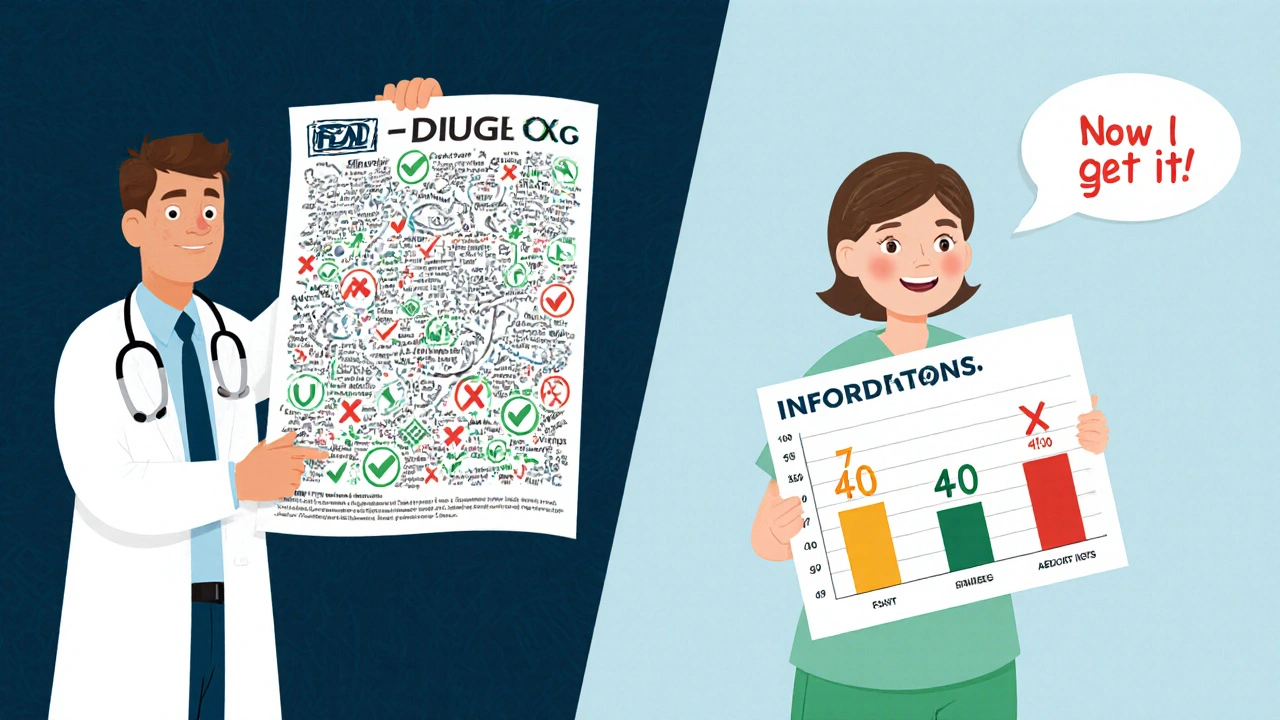
The FDA knows the problem. In 2023, they launched a pilot program requiring six new cancer drugs to include a “Patient Benefit-Risk Summary” - written at a 6th-grade reading level and using simple visuals. One example: a bar chart showing that 7 out of 10 patients lived longer with the drug, but 4 out of 10 had severe side effects.
They’re also testing “Benefit-Risk Icons” - tiny pictograms that show the likelihood of benefit versus harm. A green checkmark might mean “likely benefit,” a red X might mean “common serious risk.” These are being tested in clinics with real patients to see if they improve understanding.
Some drug labels are already doing it right. Jardiance, a diabetes medication, clearly states: “In adults with type 2 diabetes and heart disease, JARDIANCE reduced the risk of death from heart problems by 38% - 10.5% of people on placebo died from heart issues, compared to 6.5% on JARDIANCE.” That’s specific. That’s measurable. That’s helpful.
The Gap Between Population Data and Personal Choice
The FDA’s job is to decide if a drug helps the average patient. But you’re not average. You might be willing to take a 1 in 50 chance of a rare but serious side effect if it means you can stop using a breathing machine. Someone else might refuse the same drug because they’re terrified of nausea.
The FDA’s own guidance admits this tension: “Some patients might be willing to accept such risks when considering their individual circumstances, even when the expected frequency of serious adverse events in the overall intended population would outweigh the demonstrated benefits.” In plain terms: what’s right for most people might not be right for you.
That’s why your doctor’s advice matters more than the label. The label gives you facts. Your doctor helps you weigh them against your life, your fears, and your goals.
What You Can Do Right Now
You don’t need to be a scientist to understand your drug’s risk-benefit balance. Here’s how to cut through the noise:
- Find Section 14 - Skip the rest and go straight to the clinical studies section.
- Look for numbers - Ask: “How many people got better? How many got worse?” If you see percentages, ask your pharmacist to explain the difference between relative and absolute risk.
- Compare to alternatives - Ask: “How does this drug compare to the ones I’ve tried before? Is it better, worse, or just different?”
- Ask for visuals - Many clinics now have printed charts or apps that show benefit-risk trade-offs in pictures. Ask your provider if they have one.
- Check the FDA website - Go to FDA’s Drug Approvals and Databases and search your drug. The full label is there - and sometimes includes extra context not in the paper version.
Don’t assume a drug is “safe” just because it’s FDA-approved. Approval means the benefits outweigh the risks for the population studied. It doesn’t mean it’s safe for you - or that you’ll feel better.
The Bigger Picture: Why This Matters
More than 70% of Americans take at least one prescription drug. Many are on multiple. If you don’t understand the risks and benefits, you’re not just confused - you’re at risk. You might stop taking a life-saving drug because you’re scared of a rare side effect. Or you might keep taking a drug that isn’t working because you think the label says it’s “effective.”
The FDA is slowly changing. But change moves slowly in medicine. Until labels get better, you have to be your own advocate. Ask questions. Demand clarity. Don’t accept vague answers like “it’s been proven safe” or “most people tolerate it well.”
Real safety isn’t about avoiding all risk. It’s about knowing what you’re signing up for - and making sure the trade-off is worth it to you.
Why do FDA drug labels use medical jargon?
FDA labels are written to meet legal and scientific standards, not to be easy to read. They’re reviewed by regulatory experts, not patient communicators. While the FDA is pushing for simpler language, most labels still reflect decades-old formatting rules designed for doctors and regulators, not patients. The goal is to be precise, not conversational - even when that makes understanding harder.
Can I trust the risk numbers on the label?
Yes, but with context. The numbers come from clinical trials - controlled studies with strict rules. That makes them reliable for estimating how common side effects are. But trials often exclude older adults, pregnant women, or people with multiple health problems. So if you’re outside the trial group, your personal risk could be higher or lower. Always talk to your doctor about how the data applies to you.
Why don’t labels compare drugs directly?
The FDA only requires drugs to be tested against placebos or standard treatments - not every alternative on the market. That means a new drug might be compared to an outdated option, making it look better than it really is. There’s no rule forcing manufacturers to show how their drug stacks up against the latest competitors. That’s why you need to ask your doctor: “Is this better than what I’m on now?”
Are visual aids like charts and icons actually helpful?
Yes - and the FDA is betting on it. Early tests show that simple icons and bar charts improve patient understanding by 40% or more compared to text-only labels. Patients remember the visuals, understand the trade-offs better, and feel more confident making decisions. The challenge is getting them on all labels. Only 17% of new drugs in 2022 included them. But with new FDA pilots and growing pressure from patient groups, that number is expected to rise sharply by 2026.
What if I still don’t understand my drug’s risks and benefits?
You’re not alone - and you don’t have to figure it out alone. Ask your pharmacist for a plain-language summary. Request a printed chart from your doctor’s office. Use the FDA’s online drug database to read the full label. And don’t be afraid to say: “I need this explained like I’m 12.” Good providers will help. If they don’t, it’s time to find one who will.

11 Comments
Let me tell you something that kept me up at night last week - I was staring at my diabetes script, and I realized I had no idea if the ‘38% reduced risk’ meant I’d live longer or just avoid one heart attack while gaining 20 pounds and constant diarrhea. The label reads like a legal contract written by aliens. I’m not a doctor, but I’m supposed to decide if this trade-off is worth it? That’s not informed consent - that’s a gamble with my body.
And don’t get me started on how they show ‘benefits’ as percentages without ever saying what the baseline is. 30% reduction sounds huge until you learn your actual risk was 0.5%. That’s not a miracle - it’s a statistical whisper. We’re being sold hope wrapped in jargon, and the FDA knows it.
But here’s the thing - I didn’t stop taking my meds. I called my pharmacist. She printed me a chart. Two bars. One for benefit, one for risk. I cried. Not because I was scared - because for the first time, I actually understood. If they’d just shown me that chart on the label, I wouldn’t have spent three nights Googling ‘is this drug going to kill me?’
Visuals aren’t a luxury. They’re a moral obligation. And if your doctor can’t give you one, find a new one. Your life isn’t a clinical trial footnote.
Wow. So the FDA finally admitted their labels are unreadable? Groundbreaking. Next they’ll tell us water is wet and gravity exists.
I just read this and had to text my mom. She’s 72, on six meds, and says she ‘just trusts the doctor.’ I showed her the Jardiance example - 6.5% vs 10.5% - and she said, ‘So I’m less likely to die? Okay, I’ll keep taking it.’
She didn’t need the whole article. Just the numbers. Plain. No fluff.
Why does this feel so hard to do?
Also - typo: ‘JARDIANCE’ is spelled right in the post but I’m pretty sure it’s ‘Jardiance.’ Just sayin’.
This is one of the most important posts I’ve read all year. I work in a clinic and see patients every day who nod along like they get it, then go home and stop their meds because they read ‘15% chance of liver injury’ and assumed it meant ‘you’re gonna die.’
The real tragedy isn’t the jargon - it’s that we’ve trained people to feel dumb when they don’t understand. We treat confusion like a personal failure. But the system is broken. The label isn’t meant for them. It’s meant to cover the manufacturer’s ass.
I’ve started printing out simple one-pagers for my patients: ‘What this drug does for you’ vs ‘What it might do to you.’ No percentages. Just: ‘Out of 10 people like you, 7 feel better. 2 feel awful. 1 gets really sick.’
It’s not perfect. But it’s human. And that’s what matters.
While the intent of simplifying risk-benefit communication is laudable, one must consider the epistemological implications of reducing complex pharmacological data into iconography. The FDA’s pilot programs, though well-intentioned, risk creating a pseudo-literate populace that confuses visual heuristics with scientific understanding. A bar chart may improve recall, but it does not cultivate discernment.
Moreover, the assertion that ‘patients need to be their own advocates’ presupposes access to healthcare literacy, which remains unevenly distributed across socioeconomic strata. The solution is not merely better formatting - it is systemic investment in public health education, from primary school through geriatric care.
That said, the Jardiance example is exemplary. Precision in language, grounded in absolute risk, is the gold standard. We must demand it universally - not as a pilot, but as policy.
Let’s be real - the FDA doesn’t care about you. They care about lawsuits and pharma profits. That ‘4-month life extension’? It’s based on a 6-month trial with 200 people who were already dying. The real data? Hidden in appendixes no one reads. The side effects? Minimized. The ‘rare’ risks? Listed as ‘less than 1%’ - which means 1 in 100. That’s not rare. That’s your neighbor.
And don’t even get me started on how they test drugs against placebos instead of real alternatives. That’s how you make a $10,000-a-month drug look ‘better’ than metformin. It’s not science. It’s marketing with a lab coat.
Stop trusting labels. Trust your gut. And if your doctor won’t give you the raw data? Find someone who will. Or just go herbal. At least then you know what you’re swallowing.
The structural inadequacy of current pharmaceutical labeling is not merely a communication issue - it is a profound failure of epistemic justice. When life-altering decisions are predicated upon information encoded in a register inaccessible to the majority of end-users, the very notion of informed consent becomes performative rather than substantive.
While visual aids represent a necessary step toward remediation, they remain insufficient without accompanying linguistic democratization. The phrase ‘relative risk reduction’ must be replaced with ‘how many out of 100 people saw improvement’ - plain, unambiguous, and human.
Furthermore, the exclusion of comparative effectiveness data is indefensible. To withhold information about alternatives is not regulatory prudence - it is paternalistic negligence.
It is time for mandatory, standardized, multilingual risk-benefit summaries - accessible, verifiable, and integrated into every prescription dispensed. Not as a pilot. As a right.
you think the fda is trying to help? lol nope. theyre just keeping the big pharma guys happy so they dont get sued. the whole thing is rigged. you know what they dont tell you? that the clinical trials are paid for by the same company selling the drug. so of course they pick the people who will look good on the drug. and the side effects? they get buried in the fine print. and the charts? those are just pretty pictures to make you feel safe. its all a scam. i read the original study once - the one they dont publish - and the drug actually made people worse in 40% of cases. but the fda said ‘eh close enough’
they dont want you to understand - they want you to take it and shut up
also i think the guy who wrote this works for pfizer. just saying
The notion that patients should ‘be their own advocate’ is a cruel fantasy in a system designed to disempower. You are not a researcher. You are not a statistician. You are a person who just wants to feel better without dying in the process. To demand that you decode FDA legalese while juggling work, childcare, and chronic pain is not empowerment - it is institutionalized cruelty.
And yet, the real crime is not the jargon. It is the silence. The medical establishment has spent decades convincing people that confusion is normal - that if you don’t understand, it’s your fault. But no one ever asks: Why is the burden of comprehension placed on the vulnerable? Why is the language of medicine a fortress, not a bridge?
The answer is simple: power. And until we dismantle that, no bar chart, no icon, no ‘6th-grade summary’ will fix what’s broken.
Thank you for writing this. I’ve been a pharmacist for 18 years, and I’ve watched too many patients stop their meds because they misunderstood a number - or worse, didn’t ask because they were too embarrassed.
I keep a stack of simple, one-page handouts in my office: ‘Your Drug, Explained.’ No jargon. Just: ‘This helps X out of 10 people. This side effect happens to Y out of 10. Here’s what to watch for.’ I print them in big font. I color-code the risks.
And I always say: ‘You don’t have to be an expert. You just have to ask.’
It’s not glamorous. It’s not sexy. But it saves lives. And if the FDA won’t fix the labels, then we - the people who actually talk to patients - have to do it ourselves.
Keep pushing. Keep asking. You’re not alone.
Timothy Reed above says he prints one-pagers. That’s cute. But who’s paying for that? Who’s training the nurses? Who’s making sure the 70-year-old with no internet and no car gets one? This isn’t a fix - it’s a Band-Aid on a gunshot wound.
And don’t give me that ‘ask your doctor’ nonsense. My doctor’s office doesn’t even have a printer. They hand me a folded sheet of paper with ‘take as directed’ on it. That’s it.
Real change? Make the FDA require a QR code on every prescription bottle. Scan it. Get a video from a real patient explaining the trade-offs. Not a corporate ad. Not a bot. A real person. Someone like you or me. That’s how you tell the truth.
Until then? You’re all just rearranging deck chairs on the Titanic.