DRESS syndrome isn’t just a bad rash. It’s a full-body emergency that can sneak up weeks after you start a new medication. You might feel tired, develop a fever, and notice red, blotchy skin - things that look like the flu or a common virus. But if you’ve taken a drug like allopurinol, carbamazepine, or sulfamethoxazole in the past 2 to 8 weeks, this could be something far more dangerous. DRESS - Drug Reaction with Eosinophilia and Systemic Symptoms - kills about 1 in 10 people who get it. The good news? If caught early, survival rates jump to over 95%.
What DRESS Actually Looks Like
DRESS doesn’t start with a blister or peeling skin like Stevens-Johnson Syndrome. It starts quietly. You might wake up with a low-grade fever, sore throat, or swollen glands. A few days later, a rash appears - usually a widespread, flat, red, measles-like pattern covering your chest, back, and arms. It itches, but it’s not the worst part.
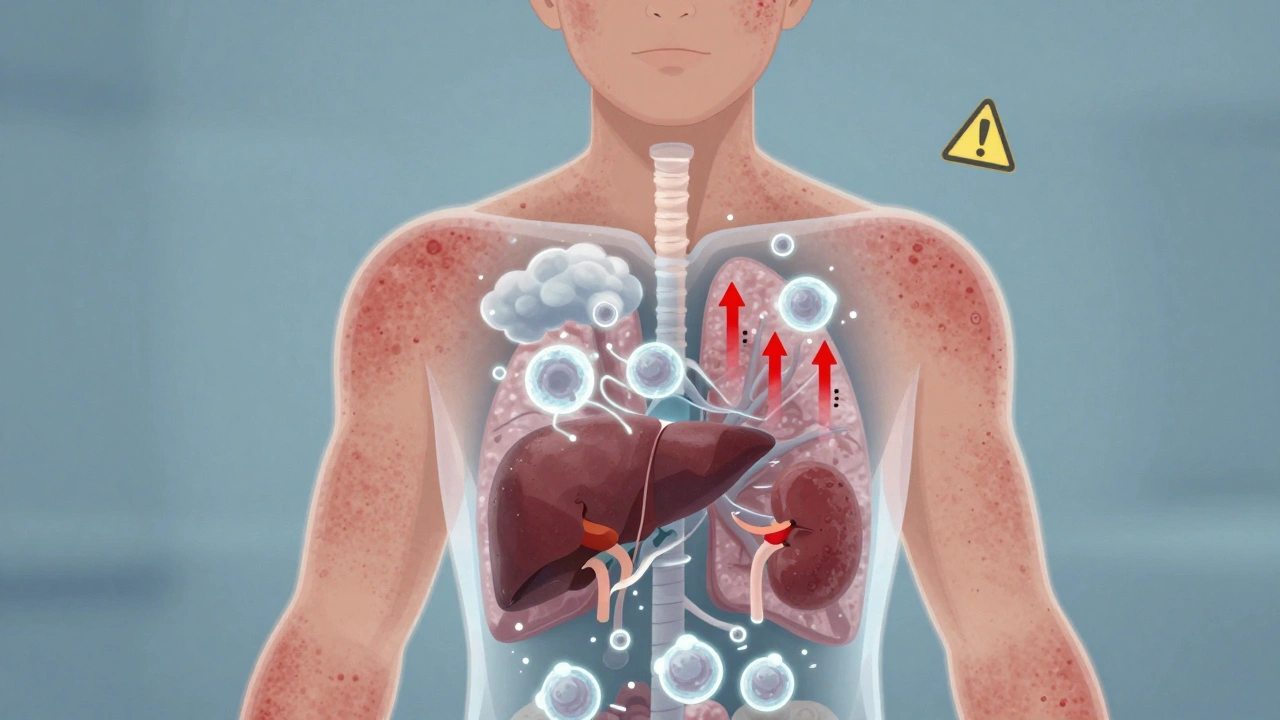
The real danger is what’s happening inside. Blood tests show eosinophils - a type of white blood cell - spiking above 1,500 per microliter. That’s more than double the normal range. At the same time, your liver enzymes (AST and ALT) can skyrocket to over 1,000 U/L. In 7 out of 10 cases, your liver is damaged. In 1 in 4, your kidneys start failing. Your lungs might fill with fluid. Your heart can get inflamed. This isn’t a skin problem. It’s a systemic immune meltdown.
Which Drugs Trigger DRESS?
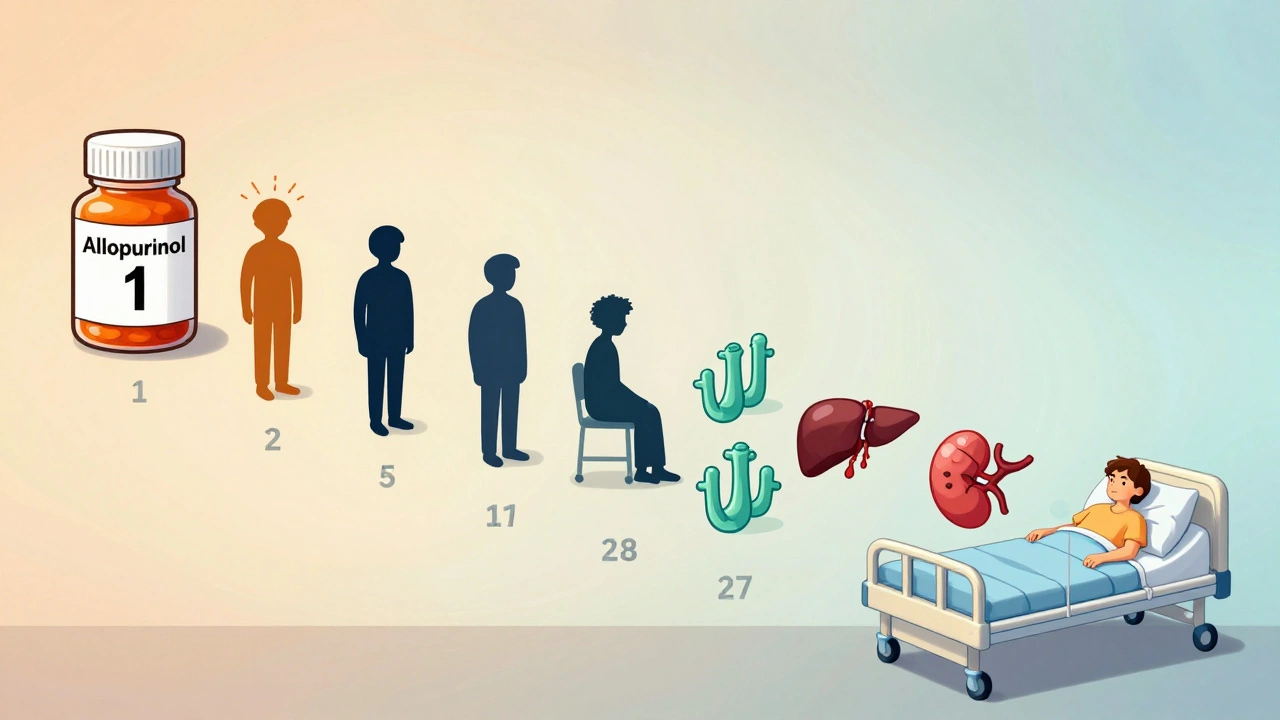
Not every drug causes this. But some are known culprits. Allopurinol - the common gout medication - is responsible for nearly half of all DRESS cases. The risk jumps dramatically if you have kidney disease. In fact, if your kidney function is below 60 mL/min, your chance of developing DRESS from allopurinol is 1 in 200.
Antiseizure drugs like carbamazepine, phenytoin, and lamotrigine cause another 20-30% of cases. Sulfonamide antibiotics - like Bactrim - are another common trigger. Even some antivirals and NSAIDs have been linked, though less often.
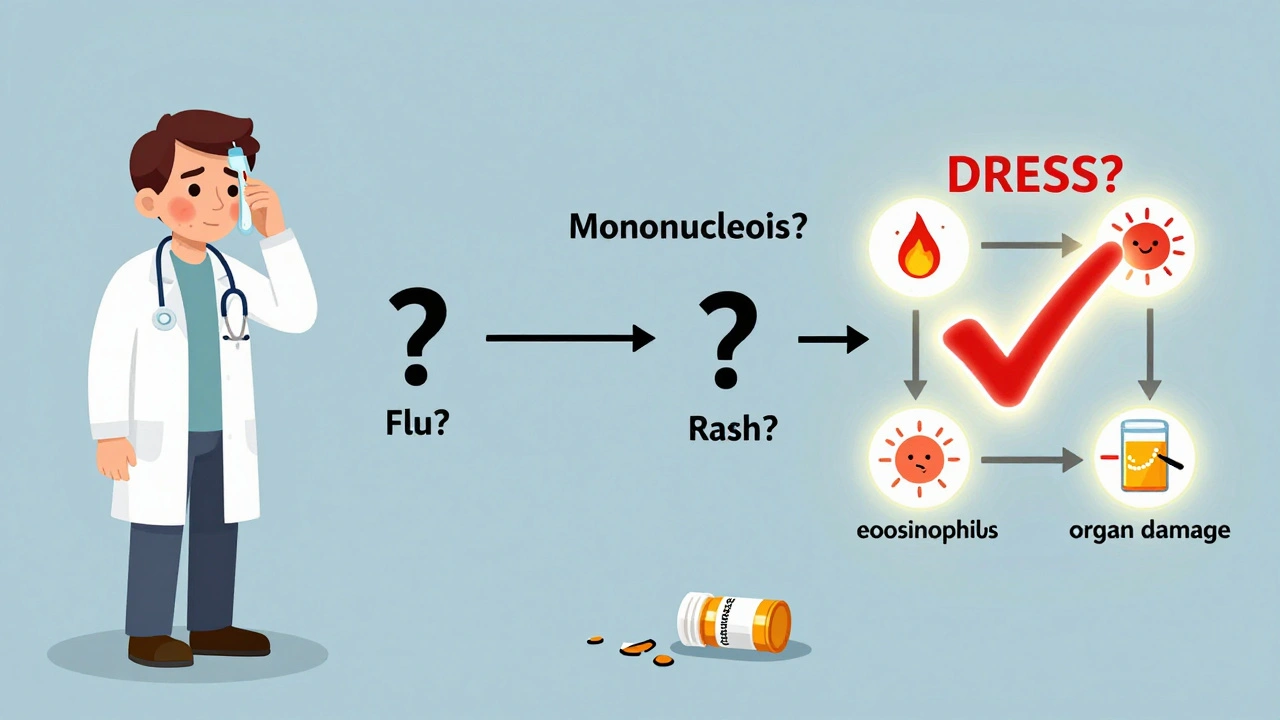
Here’s the catch: DRESS doesn’t happen right away. It takes time. Most people start feeling sick 3 to 6 weeks after beginning the drug. That’s why it’s so often missed. A doctor might think it’s a viral infection, a flu bug, or even mononucleosis. But if you’ve been on one of these drugs and now have fever, rash, and swollen lymph nodes - don’t wait. Get tested.
DRESS vs. Other Drug Reactions
It’s easy to confuse DRESS with other serious skin reactions like Stevens-Johnson Syndrome (SJS) or Toxic Epidermal Necrolysis (TEN). But they’re different in key ways.
- Latency: SJS/TEN show up within 1-4 weeks. DRESS takes 2-8 weeks.
- Skin damage: SJS/TEN cause large areas of skin to peel off. DRESS doesn’t. The skin stays mostly intact.
- Mucous membranes: SJS/TEN almost always affect the mouth, eyes, or genitals. DRESS does - but only in about half of cases.
- Blood markers: SJS/TEN don’t cause eosinophilia. DRESS almost always does.
- Organ damage: DRESS attacks the liver, kidneys, and lungs. SJS/TEN mostly stay on the skin and mucous membranes.
And then there’s HHV-6 - human herpesvirus 6. In 60-70% of DRESS cases, this virus reactivates about 2-4 weeks after symptoms start. It’s not the cause, but it makes things worse. It can prolong the illness, trigger new rashes, and even lead to long-term complications like thyroid disease or diabetes.
Why Diagnosis Is So Hard
A 2020 study found that only 35% of internal medicine residents could correctly identify a DRESS case. That’s not because they’re untrained - it’s because the signs are vague and delayed. One patient in a 2022 case report saw five different doctors over six weeks before someone finally tested for eosinophilia and liver enzymes. By then, her AST was at 2,840 U/L - nearly 100 times normal.
Doctors often miss DRESS because they’re looking for something obvious: blistering, peeling, or a clear drug allergy history. But DRESS hides in plain sight. It looks like the flu. It looks like mononucleosis. It looks like a drug rash that’s just "taking longer to clear."
That’s why the RegiSCAR criteria matter. To diagnose DRESS, you need:
- Hospitalization
- Acute rash
- Fever over 38°C
- Swollen lymph nodes
- Eosinophilia >1,500/μL or >10%
- Atypical lymphocytes
- Involvement of at least three internal organs
If you have at least three of those - especially with a recent drug exposure - it’s DRESS until proven otherwise.
What Happens If You Don’t Act Fast
Delaying treatment isn’t just risky - it’s deadly. If the drug isn’t stopped within 24 hours of symptom onset, the death rate jumps from 5% to 15%. Why? Because the immune system keeps attacking your organs even after you stop the drug. Eosinophils keep releasing toxins. The liver keeps failing. The kidneys keep shutting down.
And it doesn’t end when the rash fades. About 20-30% of survivors develop permanent organ damage. One in five needs ongoing kidney care. One in 10 develops an autoimmune disorder like Graves’ disease or lupus months after recovery. A Reddit user in 2023 described being diagnosed with type 1 diabetes five weeks after his DRESS episode resolved. That’s not rare. It’s expected.
How It’s Treated
The first step is simple: stop the drug. Immediately. No exceptions. Even if you think it’s "just a rash," if it’s DRESS, that drug is poisoning you from the inside.
Then comes hospitalization. Most patients need 14 to 21 days in the hospital. Some end up in intensive care. Treatment usually includes:
- High-dose corticosteroids - like prednisone or methylprednisolone - at 0.5 to 1 mg per kg per day
- Gradual tapering over 4 to 8 weeks to avoid rebound inflammation
- Daily blood tests: liver enzymes, kidney function, eosinophil count
- Antibiotics or antifungals if secondary infections develop (common with broken skin and weakened immunity)
- HHV-6 PCR testing to track viral reactivation
Newer treatments are showing promise. In 2022, a study showed that adding anakinra - an IL-1 blocker used for arthritis - cut hospital stays from 18.5 days to 11.2 days. Clinical trials are now testing tocilizumab (an IL-6 blocker) for patients who don’t respond to steroids.
Who’s at Risk?
Not everyone who takes allopurinol gets DRESS. But some people are genetically wired for it. If you’re of Asian descent - especially Han Chinese, Thai, or Korean - and you carry the HLA-B*58:01 gene, your risk is 55 times higher. That’s why Taiwan started screening for this gene before prescribing allopurinol. Since 2020, DRESS cases from allopurinol dropped by 75% there.
People with chronic kidney disease are also at higher risk. If your eGFR is below 60, your kidneys can’t clear allopurinol properly. The drug builds up. The immune system goes haywire. That’s why the American College of Rheumatology now recommends febuxostat as the first-choice gout medication for anyone with kidney problems.
What You Can Do
If you’re on allopurinol, carbamazepine, lamotrigine, or a sulfa drug:
- Know the warning signs: fever, rash, swollen glands, fatigue
- Ask your doctor if you should be tested for HLA-B*58:01 - especially if you’re Asian
- If you develop a rash after starting a new drug, don’t wait. Get blood work done - especially eosinophil count and liver enzymes
- Keep a list of all medications you’ve taken in the last 8 weeks - this helps doctors connect the dots
If you’ve had DRESS before, never take the same drug again - or anything in the same class. Cross-reactivity is common. A patient who had DRESS from carbamazepine might react to phenytoin or oxcarbazepine. Keep a medical alert card or bracelet.
The Bigger Picture
DRESS is rare - about 1 in 10,000 drug exposures. But with aging populations and rising use of high-risk drugs like allopurinol for mild gout, cases are expected to rise 25% by 2030. Better screening, earlier diagnosis, and new treatments are helping. But awareness is still the biggest weapon.
This isn’t a condition you can treat at home. It’s not a rash you can ignore. It’s a medical emergency that hides behind common symptoms. If you’ve been on a high-risk drug and feel off - fever, rash, tired - get tested. Fast. Your life might depend on it.


8 Comments
DRESS is one of those conditions that flies under the radar until it’s almost too late. I’ve seen it in the ER a few times - patients come in thinking it’s a virus, and by day 10, their liver’s failing. The key is knowing the timeline: if you started a new med 3-6 weeks ago and now have a rash + fever, don’t wait for the skin to peel. Get the eosinophil count and liver enzymes. That’s it. No guesswork. Stop the drug immediately. No exceptions. This isn’t a "maybe" situation.
allopurinol is the worst. i had a cousin who got it after taking it for gout. doc said "its just a rash" for 3 weeks. by the time they tested he was in icu. liver at 3k. kidney done. now he needs dialysis. why dont they warn people better?
This post reads like a medical textbook written by someone who’s seen too many dead patients. I get the urgency, but the fear-mongering is excessive. Most people take allopurinol their whole life and never have an issue. If you’re going to scare people, at least give them real stats - not cherry-picked case reports.
Oh please. Another "trust the system" post. Did you know the FDA approved allopurinol in 1966 without any genetic screening? And now they want you to believe this is about "awareness"? Wake up. Big Pharma doesn’t want you to know that a $2 blood test could prevent 90% of these deaths. They profit from dialysis, transplants, and lifelong steroids. DRESS isn’t rare - it’s covered up.
Sylvia’s comment is dangerously misleading. The incidence of DRESS with allopurinol in high-risk populations is well-documented in NEJM and JAMA - it’s not fearmongering, it’s evidence-based medicine. The 1 in 200 risk for those with eGFR <60 isn’t cherry-picked; it’s from a 2018 multicenter cohort study. And yes, HLA-B*58:01 screening in Taiwan reduced DRESS cases by 75%. That’s not conspiracy - that’s public health success. Ignoring this isn’t skepticism, it’s negligence.
I’m a nurse who’s seen 3 DRESS cases in 5 years. One patient was 22, healthy, took carbamazepine for migraines. Woke up with fever, rash, swollen neck - thought it was mono. Two weeks later, he was in the ICU with liver failure. They almost lost him. I’ve told my friends: if you’re on any of these meds and feel off, don’t Google it. Go to urgent care and ask for eosinophils and LFTs. That’s it. No drama. Just facts. Save yourself.
Wait so if i take bactrim and get a rash its DRESS? what if i just have allergies? and why is hhv-6 suddenly the villain? last week it was mold, before that it was 5g networks. this whole thing feels like medical theater. also i think the author is just trying to sell a book.
Dear Medical Community,
It is with profound concern that I address the systemic failure in pharmacovigilance that permits the continued widespread prescription of allopurinol to individuals with compromised renal function, despite the existence of validated genetic screening protocols since 2010. The reactivation of HHV-6 in 60-70% of DRESS cases is not coincidental - it is a biomarker of immune dysregulation orchestrated by undisclosed pharmaceutical lobbying interests. The RegiSCAR criteria, while statistically valid, were developed by institutions funded by the American College of Rheumatology, whose members hold patents on steroid protocols. I urge you to demand full transparency, independent replication, and the immediate suspension of all non-screened allopurinol prescriptions. Your silence is complicity.
Sincerely,
Nikki Smellie, Ph.D. (Honorary), Independent Bioethics Researcher