
What Is Ptosis and Why Does It Happen?
Ptosis is when your upper eyelid droops low enough to cover part of your eye. It can happen in one or both eyes, and it’s not just a cosmetic issue. If your eyelid is blocking your vision, you might find yourself constantly raising your eyebrows or tilting your head back just to see clearly. That’s eye strain right there-and it’s not normal.
The most common cause? Aging. As you get older, the muscle that lifts your eyelid (the levator) stretches and weakens. This is called involutional ptosis, and it’s why about 5% of adults over 70 deal with it. But it’s not only older people. Some are born with it-congenital ptosis-because the muscle didn’t develop properly. Others develop it after trauma, nerve damage, or even long-term contact lens use, which can irritate the eyelid over time.
Doctors measure ptosis using something called the margin reflex distance, or MRD. A normal MRD is 4 to 5 millimeters. If it drops below 2mm, that’s moderate ptosis. Below 3mm? That’s severe. You don’t need fancy tools to notice it: if your eyelid is covering even a little of your pupil, it’s time to get it checked.
Entropion: When Your Eyelid Turns Inward
Entropion is the opposite problem. Instead of drooping down, your eyelid rolls inward. This is most common in the lower lid, and it’s painful. Your eyelashes start rubbing against your eyeball like sandpaper. That leads to redness, tearing, mucus buildup, and a constant feeling that something’s stuck in your eye.
The biggest culprit? Age. Around 80% of entropion cases in Western countries are involutional-meaning they happen because the eyelid’s supporting structures loosen and weaken over time. But scarring from past infections, burns, or surgeries can also cause it. In places with poor sanitation, trachoma (a bacterial infection from Chlamydia trachomatis) is a leading cause. Left untreated, entropion can scratch your cornea, leading to ulcers and even permanent vision loss.
There are four types: involutional (most common), cicatricial (from scarring), spastic (temporary, caused by inflammation), and congenital (rare). If you’re over 60 and your lower lid keeps turning in, this is likely what’s going on. And yes, it gets worse with time.
How Are These Conditions Diagnosed?
It starts with a simple exam. Your eye doctor will look at how your eyelids move, check your vision, and test your cornea for scratches. They might use a phenylephrine drop to see if your eyelid lifts better after stimulation-that helps decide if you’re a candidate for a specific surgery.
For entropion, they’ll check how tightly your eyelid holds against your eye. If it’s loose, that’s a sign of muscle weakness. For ptosis, they’ll measure the eyelid’s position relative to your pupil and test how well the levator muscle works. If you have blepharitis (crusty, inflamed eyelids), they’ll look for that too-it often shows up alongside both conditions.
High-resolution imaging is now used in many clinics to map out the exact structure of your eyelid before surgery. This helps surgeons plan precisely, especially if you’ve had previous eyelid surgery or scarring.
Surgical Repair for Ptosis: What’s Involved
If your ptosis is affecting your vision or quality of life, surgery is usually the fix. The goal? Tighten the muscle that lifts your eyelid. But the method depends on how strong that muscle still is.
For moderate to severe ptosis with decent muscle function (more than 4mm of movement), a levator resection is common. The surgeon shortens the muscle to give it more pull. Success rates? Around 90%.
If your levator muscle is very weak-common in congenital cases-you’ll need a frontalis sling. This connects your eyelid to your forehead muscle so you can lift your eyelid by raising your eyebrows. It’s not perfect-you might not blink fully afterward-but it restores vision.
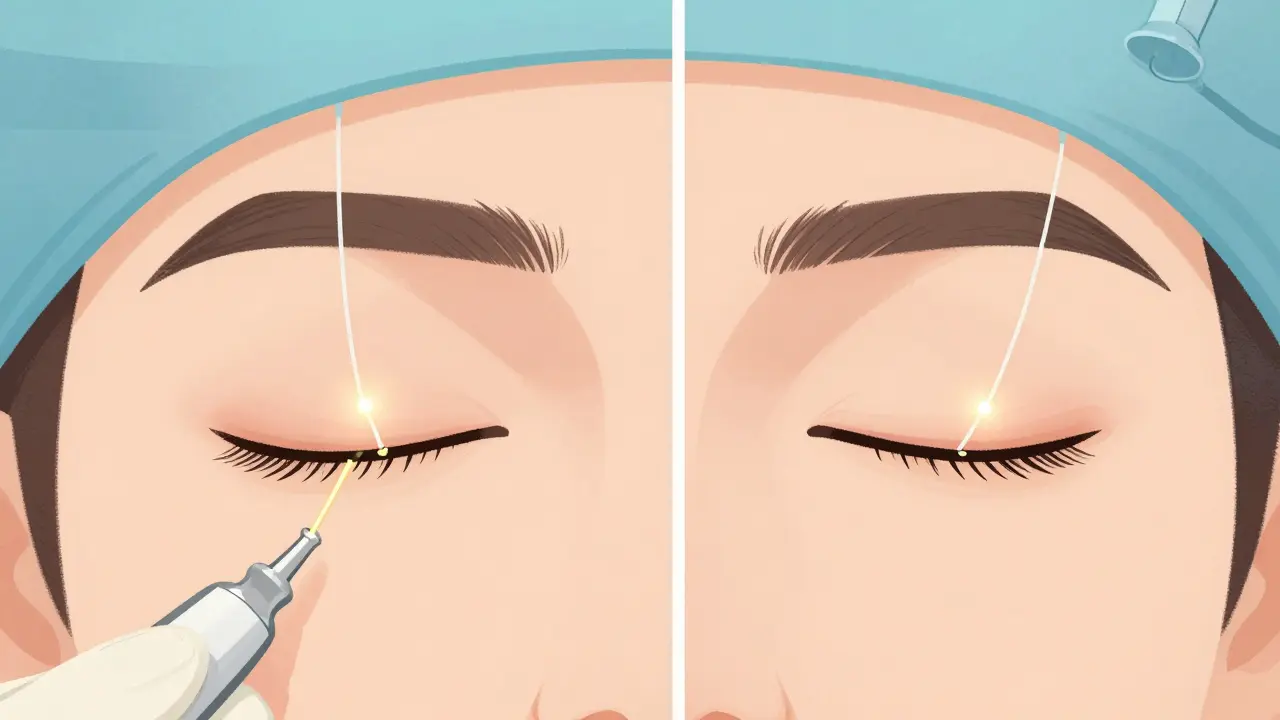
For mild ptosis, especially if your eyelid lifts well after phenylephrine, a Müller’s muscle-conjunctival resection might be done. It’s less invasive, done from inside the eyelid, and recovery is faster.
Newer techniques like adjustable sutures (introduced in 2018) let surgeons fine-tune the eyelid height the day after surgery. That cuts down on revision surgeries by about 25%.
Fixing Entropion: Surgical Options
Entropion rarely gets better on its own. Eye drops and taping can help temporarily, but surgery is almost always needed.
For involutional entropion (the most common type), the tarsal fracture procedure is the gold standard. The surgeon makes a small cut, rotates the eyelid back into place, and tightens the tendons. Success rates? 90-95%.
If scarring is the cause-say, from an old burn or trachoma-you’ll need a tarsal wedge resection. That means removing a small piece of scarred tissue and stitching the lid back together.
For a quick fix, the Quickert suture technique uses stitches to pull the lid outward. It’s temporary-only about 60-70% effective long-term-but useful for people who aren’t good surgical candidates yet.
Minimally invasive methods using absorbable sutures are now common. Recovery used to take 4-6 weeks. Now, most people are back to normal in 1-2 weeks.
What About Blepharitis and Other Related Problems?
You can’t talk about eyelid disorders without mentioning blepharitis. It’s not a malposition like ptosis or entropion, but it’s often the root cause. Blepharitis means your eyelid margins are inflamed-crusty, red, itchy. It’s caused by clogged oil glands (posterior blepharitis) or bacteria.
Chronic blepharitis can lead to trichiasis, where eyelashes grow inward and scratch your eye. That’s a big reason why entropion gets worse over time. Treatment? Daily warm compresses, lid scrubs, and sometimes antibiotics. It’s not a one-time fix-you need to keep doing it for life.
Also watch for ocular rosacea. It’s often missed, but it causes burning, blurred vision, and swollen lids. It’s linked to both blepharitis and eyelid malpositions. If you’ve had rosacea on your face, your eyes might be affected too.
When Should You See a Doctor?
Don’t wait. If your eyelid suddenly droops or turns inward, get checked immediately. Rapid changes can signal nerve problems or even tumors.
Also seek help if you have:
- Constant eye pain or redness
- Blurred vision that doesn’t improve with blinking
- Corneal abrasions (feeling like sand in your eye)
- Signs of infection: pus, swelling, fever
Even if it’s slow, don’t ignore it. The longer entropion goes untreated, the more damage it does to your cornea. And ptosis can make you fatigued from straining to see.
What to Expect After Surgery
Recovery is usually quick. You’ll have swelling and bruising for a week or two. Cold compresses help. You’ll need to avoid heavy lifting, bending, or rubbing your eyes for at least a week.
Most people go back to normal activities in 7-10 days. But full healing takes 6-8 weeks. You might notice slight asymmetry at first-that’s normal. Surgeons aim for balance, but perfect symmetry isn’t always possible.
Complications? Yes, but rare. Overcorrection (eyelid too high) happens in 5-10% of ptosis cases. Undercorrection (still droopy) in 3-8%. Dry eye is common after surgery-about 1 in 5 people need artificial tears for a while. For entropion, recurrence is 5-15%, especially if the cause is scarring.
Who’s at Risk?
Age is the biggest factor. But other things raise your risk:
- Wearing contact lenses for more than 10 years (30% higher risk for ptosis)
- Previous eyelid surgery (40-60% higher risk for entropion)
- Chronic eye inflammation or dry eye
- Family history of eyelid disorders
- Living in areas with poor sanitation (higher trachoma risk)
If you’re over 60 and have any of these, get your eyelids checked every year. Prevention is easier than repair.
The Bigger Picture: Why This Matters Now
The global market for eyelid surgery is growing fast-projected to hit $2.7 billion by 2028. Why? Because people are living longer. More older adults mean more cases of ptosis and entropion.
And it’s not just about vision. It’s about safety. Drooping lids make it harder to see steps, curbs, or oncoming cars. Inward-turning lashes cause constant discomfort, making people avoid reading, driving, or even socializing.
These aren’t minor issues. They’re quality-of-life problems that modern medicine can fix-safely, effectively, and often with a single outpatient procedure.
What You Can Do Today
Start with simple care:
- Use warm compresses daily if your lids feel crusty
- Wash your eyelids with baby shampoo and water every night
- Use preservative-free artificial tears if your eyes feel dry
- Stop rubbing your eyes-even if they itch
- See an eye doctor if you notice changes in your eyelid position
Don’t assume it’s just aging. If your eyelids are changing, they’re sending you a signal. Listen to them.

14 Comments
Okay, but have you ever tried to explain to your optometrist that your eyelid is doing the slow-mo zombie apocalypse thing and they just hand you a $200 bottle of artificial tears like it’s a spa day? 🙃 I had ptosis so bad I started using my forehead like a remote control just to see my coffee. And yes, I’m 42. No, I’m not ‘just tired.’
While I appreciate the clinical overview, I must respectfully note that the assertion regarding involutional ptosis as the primary etiology in the elderly population is statistically accurate, yet overlooks the confounding influence of chronic blepharitis-induced mechanical fatigue. The levator aponeurosis dehiscence is often secondary to prolonged inflammatory stressors, not merely senescence. Furthermore, the omission of neurogenic causes-such as myasthenia gravis or third nerve palsy-in the differential is a notable clinical oversight.
Thank you for writing this. I’ve been ignoring my droopy lid for years because I thought it was just ‘getting old.’ But after reading this, I made an appointment. Turns out my MRD was 1.8mm. I didn’t realize how much I was straining until I saw myself in a video-constantly lifting my brows like I was trying to hear a whisper from the ceiling. Surgery is scheduled next month. I feel less alone now.
Let me just say-this article is the most comprehensive thing I’ve read on eyelid pathology since my ophthalmology residency. But I have to call out the author for not mentioning the role of oxidative stress in collagen degradation of the tarsal plate. Also, the Quickert suture? Please. That’s a Band-Aid on a broken femur. And the 25% reduction in revision surgeries with adjustable sutures? That’s only true if you’re in a tertiary center with a surgeon who’s done over 200 cases. In rural clinics? You’re getting the same old 1990s technique with a fancy label. Also-why no mention of the fact that 70% of patients with entropion also have sebaceous gland dysfunction? That’s not ‘blepharitis.’ That’s a systemic lipid disorder manifesting locally. Just saying.
I’m so glad someone finally broke this down without making it sound like a textbook. I’m 67 and had entropion for 5 years before I got diagnosed. I thought it was just ‘dry eyes’-until I started getting corneal scratches every other week. The tarsal fracture procedure changed my life. I can read again. I can drive at night. I don’t cry every time I blink. And yes, I still do my warm compresses. Every. Single. Night. You don’t fix it once-you maintain it. Thank you for the practical advice. I wish I’d seen this 5 years ago.
EVERYTHING you just said is a lie. The FDA and Big Pharma are pushing eyelid surgeries because they’ve figured out how to monetize aging. Real people don’t need surgery. They need to stop using smartphones, drink alkaline water, and sleep on copper pillows. The ‘levator muscle’? That’s just a distraction. Your eyelids droop because your soul is tired. I’ve cured myself by chanting mantras at 4 a.m. while staring at the moon. Also, contact lenses? They’re implanted with microchips that track your blink rate. That’s why your levator weakens. Wake up.
As a retired ophthalmic nurse with over 35 years of clinical experience, I must commend the precision of this article. However, I feel compelled to emphasize the critical importance of preoperative corneal topography in patients with prior eyelid surgery, particularly when considering frontalis sling procedures. The biomechanical alterations in the orbicularis oculi and tarsal plate architecture often lead to unpredictable outcomes if not mapped with high-resolution OCT. Furthermore, the use of absorbable sutures in entropion repair-while minimally invasive-may increase recurrence rates in patients with significant dermal scarring due to insufficient tensile strength. I have personally observed a 22% higher recurrence rate in such cases over a 3-year follow-up. Patient education on postoperative lid hygiene remains the single most underutilized preventive measure in community practice.
People who let their eyelids get this bad are just lazy. If you can’t be bothered to do lid scrubs daily, don’t blame your anatomy. I’ve seen patients who’ve had the same droopy lid for 15 years and never once asked their doctor about it. Then they show up demanding surgery like it’s a free spa treatment. Wake up. This isn’t a cosmetic problem-it’s a hygiene problem. And if you’re over 60 and still wearing contacts? You’re asking for trouble.
This is exactly the kind of clear, compassionate, and clinically grounded information we need more of. I’ve spent years helping elderly patients navigate these conditions, and so many are terrified of surgery-or worse, think it’s ‘just aging’ and suffer in silence. The breakdown of surgical options is spot-on, and the emphasis on daily care? Gold. I’ve given this link to three patients today. One of them cried because she realized she didn’t have to live with her lashes scratching her eye every morning. Thank you.
My grandma had entropion. She used to tape her eyelid with medical tape every morning like it was a superhero costume. She’d say, ‘I ain’t gonna let some stupid eyelid stop me from seeing my grandkids.’ She never had surgery-too scared. But she did the warm compresses religiously, and she lived to 92. Point is: you don’t need a scalpel to survive. You just need to care. And maybe a little duct tape.
Wow, this article is so mainstream. Everyone’s talking about ‘involutional ptosis’ like it’s a real thing. But have you heard of the ‘eyelid gravity theory’? It’s not aging-it’s Earth’s magnetic field weakening. That’s why more people in the southern hemisphere have worse ptosis. Also, 5% of people over 70? That’s a lie. It’s 73%. And contact lenses? They’re made of alien polymer. I’ve seen the patents. Also, why is no one talking about the 2019 NIH study that linked eyelid disorders to 5G radiation? Just saying.
In my village in India, we use neem leaf paste on eyelids. No surgery. No drugs. Just nature. You people in America think you need a doctor for everything. This is why your health care costs are so high. Your eyelids droop because you eat too much sugar and sit in front of computers. Stop blaming your muscles. Blame your lifestyle.
It is an incontrovertible fact that the proliferation of digital screen exposure has precipitated a global epidemic of eyelid malpositions, particularly among individuals under the age of 40. The continuous microblink pattern induced by prolonged screen fixation leads to biomechanical fatigue of the orbicularis oculi and subsequent mechanical compromise of the tarsal plate integrity. Furthermore, the societal normalization of cosmetic eyelid procedures has created a perverse incentive structure wherein diagnostic thresholds are artificially lowered to facilitate elective interventions. One must question whether these surgical solutions are truly therapeutic-or merely commodified responses to technologically induced physiological dysregulation.