
When a patient takes a generic pill, they expect the same effect as the brand-name version. But what if that pill doesn’t perform the same way? Increasingly, clinicians are raising red flags-not because the drug doesn’t contain the right active ingredient, but because of how and where it’s made.
Generic drugs aren’t all created equal
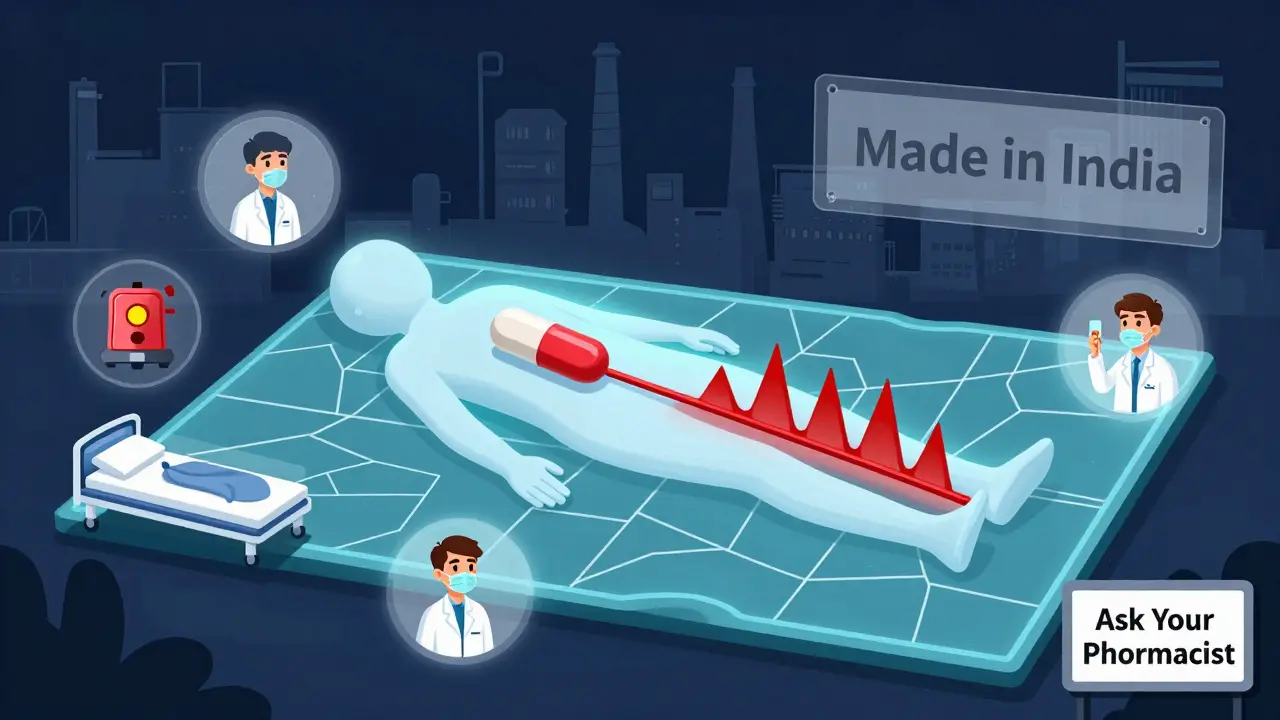
Generic drugs are supposed to be identical to brand-name drugs in active ingredients, dosage, and effectiveness. The FDA requires them to prove bioequivalence: they must deliver the same amount of medicine into the bloodstream at the same rate. On paper, that sounds solid. But in practice, the story gets messy.One major issue? Manufacturing is spread across the globe. A single generic drug might have its active ingredient made in India, mixed with fillers in China, coated in Germany, and packaged in Mexico. Only one company name appears on the label-usually a distributor, not the actual maker. That makes it nearly impossible for doctors or patients to trace where the real quality risks lie.
And here’s the kicker: the FDA inspects U.S. factories without warning. Overseas? They schedule visits months in advance. That gives manufacturers time to clean up, fix equipment, or hide problems. As one Ohio State researcher put it, it’s like showing up for a surprise audit after the company’s been told you’re coming.
Higher risk, lower cost
A 2023 study from Ohio State University looked at over 10 million adverse event reports in the FDA’s database. They compared generic drugs made in the U.S. with those made in India-and found something alarming. Indian-made generics were linked to 54% more severe adverse events, including hospitalizations, disabilities, and deaths. This wasn’t a random spike. It was consistent across multiple drugs, especially older ones that have been on the market for years.Why older drugs? Because as time passes, competition drives prices down. Companies cut corners to stay profitable. They use cheaper materials. They skip maintenance. They outsource more steps to lower-cost suppliers. The result? A drug that meets the letter of the law-but not the spirit.
Take insulin, for example. A generic version might cost $30 instead of $300. Sounds great. But if the formulation isn’t stable, or the coating dissolves too fast, blood sugar levels can swing dangerously. Clinicians have seen patients on generic insulin suddenly need emergency care-because the drug didn’t behave the way it should.
Who’s checking the checkers?
The FDA says the system works. They point to their 1,300 inspectors and say the U.S. drug supply is among the safest in the world. But their own data tells a different story. Between 2018 and 2023, over 60% of drug shortages were tied to manufacturing problems-mostly in older generics. The root cause? Outdated equipment, poor quality control, and supply chain fragility.What’s worse? Many of these factories are in countries with weaker regulatory oversight. Some don’t even have systems to track batch recalls. If a batch of metformin is contaminated, it might take months to trace it back. By then, thousands of patients could’ve already taken it.
And it’s not just about safety. It’s about reliability. When a hospital runs out of a generic antibiotic because the Indian factory had a power outage, nurses have to scramble. They switch to more expensive alternatives. They delay treatments. Patients get sicker. In cancer care, a week’s delay can mean the difference between remission and progression.

Advanced manufacturing could fix this
There’s a solution hiding in plain sight: advanced manufacturing technologies. Continuous manufacturing, real-time monitoring, and automated quality checks can catch problems before a single pill leaves the facility. These systems reduce waste, improve consistency, and cut downtime.Here’s the twist: over 80% of drugs made with these technologies are already produced in the U.S. Why? Because the upfront cost is high-millions of dollars-and foreign manufacturers of low-cost generics can’t justify it. They’re playing a different game: win by being the cheapest, not the best.
But what if the market rewarded quality instead of just price? What if hospitals and insurers paid more for generics made in facilities with verified quality systems? That’s what researchers at Ohio State are pushing for: transparency. Let patients and doctors see where a drug was made. Let them choose based on safety, not just cost.
The domestic manufacturing argument
The University of Wisconsin’s School of Pharmacy put it bluntly: if we made more generics at home, we’d have fewer shortages, fewer quality issues, and a more resilient supply chain. It’s not about nationalism. It’s about control.When a factory is in Ohio, the FDA can show up unannounced. When something goes wrong, they can act fast. When a new batch is recalled, it doesn’t get stuck in customs for weeks. Domestic production isn’t the only answer-but it’s a critical piece.
Some argue that bringing manufacturing back would raise prices. But studies show that once advanced manufacturing systems are up and running, per-unit costs actually drop. The savings come from less waste, fewer recalls, and fewer drug shortages-which cost the U.S. healthcare system over $200 billion annually.
What clinicians are seeing in real life
Dr. Iyer, a pharmacist in Texas, says he’s started asking patients: “Have you noticed any changes since switching to the generic?” Sometimes, they say their headaches got worse. Or their blood pressure became harder to control. Other times, they just feel “off.” These aren’t dramatic reactions. They’re subtle-and easily dismissed.But when multiple patients report the same thing? That’s not coincidence. That’s a signal. Clinicians aren’t anti-generic. They’re pro-safety. They want medications that work the same every time, no matter where they’re made.
One nurse in Florida told her team to stop switching patients to a new generic version of levothyroxine after three patients developed palpitations and weight loss. The FDA later confirmed the batch had inconsistent dissolution rates. The drug met bioequivalence standards-but not real-world performance.
The real question: Who’s paying the price?
We talk about saving money with generics. But we don’t talk about the hidden costs: longer hospital stays, emergency visits, missed work, and lost productivity. When a patient’s heart medication doesn’t work right, the bill doesn’t stop at the pharmacy counter.And let’s be honest: the people who pay the most aren’t the ones choosing the drug. It’s the insurance company. The hospital. The government program. The patient gets whatever’s cheapest on the formulary. They don’t get to see the inspection reports. They don’t know if the pill came from a factory with a history of violations.
It’s time to change that. Transparency isn’t just a nice idea-it’s a necessity. Doctors need to know where drugs come from. Patients deserve to know. And if we want to trust our medications, we need to stop pretending that all generics are the same.
What can you do?
If you’re a patient: if you notice a change in how a generic drug works-side effects, effectiveness, timing-tell your doctor. Keep a log. Don’t assume it’s “all in your head.”If you’re a clinician: ask your pharmacy about the manufacturer. Push for transparency. Support institutions that prioritize quality over cost. Document any unusual reactions and report them to the FDA.
If you’re a policymaker: fund inspections that are truly random, regardless of location. Incentivize domestic manufacturing with tax credits and grants. Require manufacturers to label the country of origin for APIs.
Generic drugs saved billions. But they can’t keep saving lives if we ignore the cracks in their foundation.
Are generic drugs safe if they’re made overseas?
Some are. But the risk increases significantly when manufacturing happens in countries with less transparent oversight. A 2023 study found Indian-made generics had 54% more severe adverse events than U.S.-made versions of the same drug. The FDA inspects U.S. facilities without notice-but schedules inspections in advance overseas, which can allow manufacturers to hide problems.
Why do generic drugs sometimes seem to work differently?
Generic drugs must meet bioequivalence standards, meaning they deliver the same amount of active ingredient as the brand-name version. But they don’t have to match inactive ingredients, coating, or dissolution rates exactly. Changes in these factors can affect how quickly the drug is absorbed-especially for narrow-therapeutic-index drugs like warfarin, thyroid meds, or seizure medications. Small differences can lead to big clinical effects.
Can I find out where my generic drug was made?
Not easily. Drug labels don’t list the manufacturing location. The FDA doesn’t require it. But some pharmacies and online tools now provide manufacturer information upon request. You can also report concerns to the FDA’s MedWatch program, which tracks adverse events linked to specific batches.
Why hasn’t the FDA fixed this problem?
The FDA has limited resources and faces political pressure to keep drug prices low. While they’ve started programs to promote advanced manufacturing and increase overseas inspections, progress is slow. Many of their inspection protocols haven’t changed in decades. Experts argue that unannounced global inspections and mandatory origin labeling are needed-but these require funding and legislative support.
Should I avoid generic drugs altogether?
No. Most generics are safe and effective. But if you’re taking a critical medication-like blood thinners, epilepsy drugs, or heart medications-and you notice a change in how you feel after switching generics, speak up. Ask your doctor to check the manufacturer. Sometimes, sticking with one brand or manufacturer can make a real difference in your health outcomes.






11 Comments
Let me get this straight - we’re okay with letting India manufacture half our medicine but freak out when the pills don’t work exactly the same? That’s like complaining your IKEA bookshelf wobbles after you bought it for $40. The system’s designed this way on purpose: cheap drugs, zero accountability. The FDA’s got inspectors in flip-flops doing paperwork while factories in Hyderabad pump out batches with more variance than a TikTok dance trend. And don’t even get me started on how they schedule inspections like it’s a damn yoga retreat. If you’re gonna outsource your healthcare to a country where ‘quality control’ means ‘hope for the best,’ don’t act surprised when people start dying from inconsistent dissolution rates. This isn’t a flaw - it’s the business model.
i understand your fear but let me tell you something from inside the factory where we make metformin... we work 16 hours a day under heat and pressure and still try to keep the batches consistent. yes the machines are old but we do our best. the inspectors come and they see clean floors and happy workers. they dont see the 3am shift when the power flickers or when the cooling system fails. we are not villains. we are people trying to feed our families. the problem is not us its the price they force us to sell at. if you pay more we can buy better machines. if you pay less we make do. its not about laziness its about survival
Biopharmaceutical equivalence is a statistically derived construct predicated on Cmax and AUC thresholds - but these metrics are population-level aggregates that mask inter-individual pharmacokinetic variance, particularly in narrow-therapeutic-index agents. The FDA’s bioequivalence paradigm assumes homogeneity of excipient profiles, dissolution kinetics, and polymorphic form stability - all of which are routinely compromised in global supply chains due to cost-driven substitution of non-regulated fillers, inconsistent granulation techniques, and non-validated coating processes. The consequence? Clinically significant subtherapeutic or supra-therapeutic exposure in vulnerable populations - a phenomenon empirically validated in the Ohio State cohort but systematically dismissed as ‘anecdotal’ by regulatory gatekeepers who conflate regulatory compliance with clinical safety.
Oh wow. So now we’re blaming poor countries for the fact that American corporations outsourced everything to maximize profits? That’s rich. You want safe drugs? Then stop letting CVS and Walmart choose your meds based on the lowest bid. You want transparency? Then stop letting pharmaceutical conglomerates hide behind shell companies and ‘distributors.’ You want quality? Then pay for it. Stop acting like you’re outraged when you’ve been complicit in this whole mess for 20 years. And don’t even get me started on how you all cry about insulin prices but won’t boycott the pharmacy that stocks the cheapest generics. Hypocrites.
so i talked to my buddy who works at a med supply co in indiana and he said most of the generic stuff labeled 'made in usa' actually has the active ingredient from india or china - just mixed and packaged here. the real issue is not where it's made but who's controlling the supply chain. the big pharma middlemen don't care about the factory - they care about the profit margin. and the FDA? they're understaffed and overworked. they inspect one plant every 10 years if they're lucky. the system is broken because it's designed to be broken - profit over people. but hey at least the pills are cheap right? 😅
i’ve been a nurse for 18 years and i’ve seen patients switch to generics and suddenly feel like crap. not dramatic stuff - just tired, dizzy, headaches. we chalked it up to aging until we noticed a pattern. one woman on levothyroxine went from stable to crashing - we switched her back to brand and she was fine in 48 hours. i wish we could see the manufacturer on the bottle. it’s not about being anti-generic. it’s about being pro-accuracy. we need better tracking. simple as that.
It is imperative to underscore, with the utmost gravitas, that the current regulatory framework governing the global pharmaceutical supply chain constitutes a fundamental dereliction of fiduciary duty to the American populace. The commodification of life-sustaining therapeutics - reduced to mere line items on a balance sheet - represents a moral and epistemological collapse of public health infrastructure. To permit the manufacturing of critical medications in jurisdictions lacking robust oversight mechanisms is not merely negligent - it is an affront to the sanctity of human life. I urge, with unyielding conviction, that immediate legislative action be taken to mandate domestic production of all Class I therapeutics, coupled with mandatory origin labeling, and the establishment of a federal pharmaceutical quality assurance corps with subpoena power and unannounced inspection authority - without exception.
my dad’s on blood thinners. switched to a generic last year. started getting nosebleeds. didn’t say anything for months ‘cause he didn’t wanna be ‘that guy.’ finally told his pharmacist - turns out the new batch was from a different factory. switched back to the old one, nosebleeds stopped. no one told him the manufacturer changed. no one even asked. we’re supposed to just trust that the pill in the bottle is the same as last month? that’s insane. we need a barcode or something. scan it, see where it came from. simple. why isn’t this a thing yet?
i know this sounds crazy but i think the FDA is being controlled by big pharma to keep prices low so people don’t revolt. they know the generics are risky but they let it slide because if people found out how bad it is they’d demand real medicine and that would cost too much. i read somewhere that the same factory that made the bad metformin also made fake cancer drugs in 2019. they got fined $2 million - which is less than what they made in one week. the system is rigged. we’re all guinea pigs. and the worst part? they’re testing this on old people and poor people because they don’t have the money to fight back. i’m scared to take my pills anymore
Let’s be brutally honest here - this isn’t a quality issue, it’s a colonialist nightmare. We outsourced the dirty work to the Global South, then act shocked when the product has flaws. We demand cheaper drugs, then act morally superior when the pills don’t work. The same corporations that profit from this system are the ones lobbying against transparency. Meanwhile, Indian and Chinese workers are getting blamed for doing exactly what we paid them to do: make it cheap. The real villain? The American consumer who clicks ‘buy now’ without reading the fine print. We didn’t just break the system - we built it ourselves. And now we’re surprised it’s falling apart. Classic.
They’re putting microchips in the pills to track us. That’s why the generics feel different - the chips interfere with your nervous system. The FDA knows. The WHO knows. That’s why they won’t let you see the manufacturer. They don’t want you to know you’re being monitored. My cousin’s neighbor’s dog got sick after eating a generic pill - that’s not a coincidence. It’s the beginning of a mind control program. I’ve started buying my meds from Canada. At least they’re honest about where it’s from. You think this is about safety? No. It’s about control.