29 Dec |
11:12 AM
Medication-Food Interaction Checker
Check Your Medication's Food Interaction
Foods to Avoid:
Risks:
Important: This tool provides general information only. Always consult your pharmacist or doctor for personalized medical advice.
Many people swallow their pills with a glass of water and move on with their day-no thought given to what they ate, or didn’t eat, before or after. But that simple habit could be making side effects worse, or even making your medicine less effective. The truth is, food isn’t just something you eat. It’s a powerful player in how your body handles medication.
Why Food Changes How Medicine Works
Your stomach and intestines aren’t just digesting your breakfast-they’re also absorbing your pills. Food changes the environment inside your gut. It slows down how fast your stomach empties, alters the acid levels, and even interacts directly with drug molecules. These changes can make your medicine work better-or worse. For example, some antibiotics like ciprofloxacin can’t be absorbed properly if you’ve just eaten dairy. The calcium in milk binds to the drug and carries it out of your body before it can do its job. On the flip side, medications like griseofulvin (used for fungal infections) need fat to be absorbed at all. Take it on an empty stomach, and it might as well be water. The science behind this isn’t new. Back in the 1930s, researchers first noticed that meals changed how drugs moved through the body. Today, the FDA requires every new drug to be tested with food. In fact, 78% of medications approved between 2018 and 2023 came with specific food instructions because of what they found.How Food Cuts Down Side Effects
One of the biggest reasons to take medicine with food is to protect your stomach. Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen are notorious for causing stomach irritation. Studies show that people who take them on an empty stomach are nearly three times more likely to develop stomach ulcers than those who take them with a meal. Endoscopic exams reveal that 38% of patients on empty stomachs had visible damage to the stomach lining-only 12% did when they ate first. The same goes for metformin, a common diabetes drug. Over 60% of patients report severe nausea, diarrhea, or cramps when they take it without food. When taken with a meal, those side effects drop to under 20%. It’s not that the drug stops working-it’s that your gut has time to adjust. Even powerful drugs like methotrexate, used for autoimmune diseases and cancer, cause less nausea and vomiting when taken with food. In one Reddit thread with over 1,200 patient stories, 78% said eating helped them stick to their treatment plan because they felt less sick.When Food Makes Things Worse
It’s not always about protection. Sometimes, food makes a drug too strong-or blocks it entirely. Grapefruit juice is the most famous offender. It shuts down an enzyme in your gut called CYP3A4, which normally breaks down certain drugs before they enter your bloodstream. Without it, drugs like cyclosporine (used after organ transplants) can spike in your blood by 300-500%. One glass of grapefruit juice can do this for up to three days. That’s why doctors warn you not to even have a single glass if you’re on certain statins, blood pressure meds, or anti-anxiety drugs. Then there’s warfarin, a blood thinner. It works by fighting vitamin K, which helps your blood clot. But if you eat a salad one day and fried chicken the next, your vitamin K levels swing. That throws off your INR numbers and puts you at risk of clots or bleeding. Patients who keep their leafy greens consistent see far fewer hospital visits. And then there’s levothyroxine, the thyroid hormone replacement. This one has to be taken on an empty stomach-no coffee, no cereal, no calcium-fortified orange juice. Even a small amount of food can cut absorption by up to 55%. A Cleveland Clinic survey found that over half of patients admitted to taking it with breakfast-and nearly a third needed higher doses because their levels never stabilized.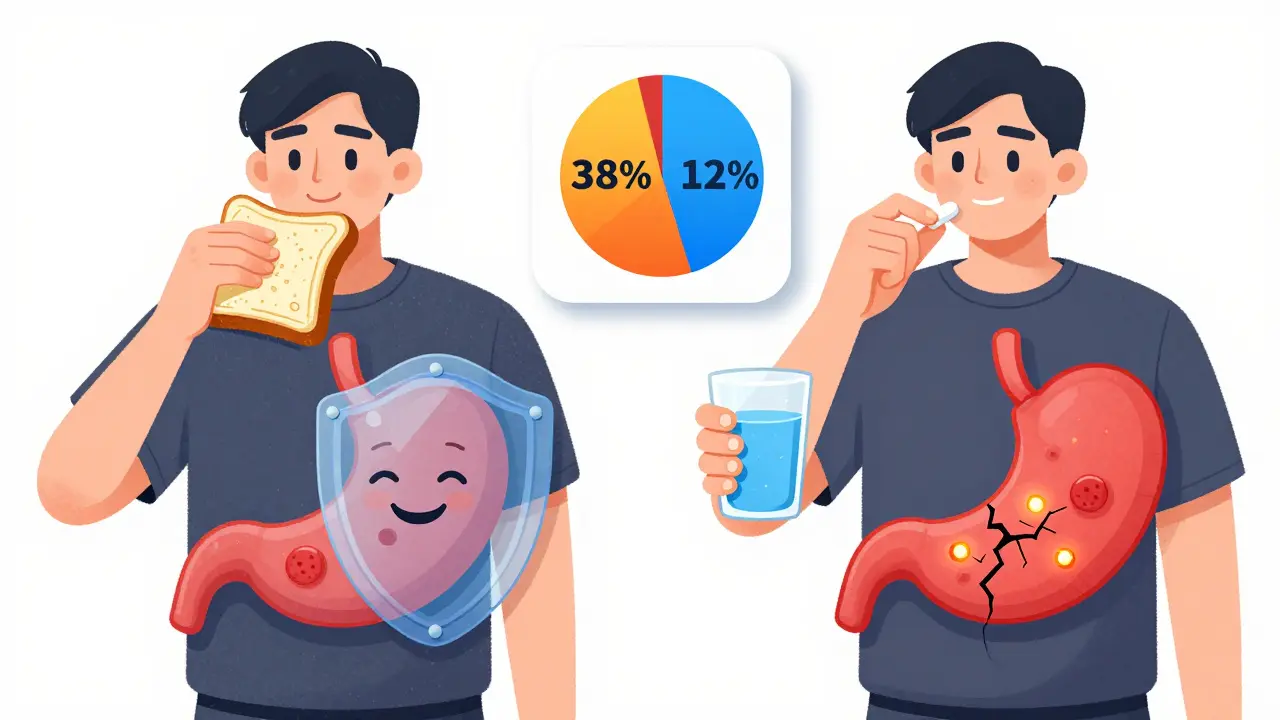
What ‘With Food’ and ‘On Empty Stomach’ Really Mean
You’ve probably seen labels like “take with food” or “take on an empty stomach.” But what does that actually look like? “Take with food” doesn’t mean a handful of crackers. The FDA defines it as at least 250-500 calories. That’s a small sandwich, a bowl of oatmeal with nuts, or yogurt with fruit. Just a sip of milk or a bite of toast won’t cut it. “Take on an empty stomach” means 1 hour before or 2 hours after eating. That’s why people taking levothyroxine are told to take it first thing in the morning, before coffee or breakfast. If you eat too soon after, your body won’t absorb enough. And timing matters. Proton pump inhibitors like omeprazole need acid in your stomach to activate. So they’re taken 30 minutes before a meal-not with it.What Happens When You Ignore the Rules
It’s easy to think, “I’ve taken this pill without food for years and I’m fine.” But side effects aren’t always immediate. Sometimes they build up. A study from the American Pharmacists Association found that 68% of medication-related hospitalizations are tied to food-drug timing mistakes. That’s not just nausea-it’s kidney damage from too much NSAID, internal bleeding from warfarin gone wrong, or toxic levels of statins from grapefruit juice. The cost? Over $177 billion a year in the U.S. alone. And it’s mostly preventable. Older adults are especially at risk. A Mayo Clinic study found that 68% of patients over 65 didn’t know the food rules for their meds. And only 22% had been told by their doctor. Most just read the label-assuming it meant “try to take it with food if you can.”How to Get It Right
You don’t need to memorize every interaction. Here’s how to stay safe:- Ask your pharmacist every time you get a new prescription. Don’t assume the rules are the same as your last drug.
- Use a pill organizer with time slots. Some apps like Medisafe send reminders for food timing too.
- Keep a simple food log if you’re on warfarin, thyroid meds, or antibiotics. Note what you ate and when you took your pills.
- Look for color-coded charts from your pharmacy. Many now label meds as “must take with food,” “must take empty,” or “flexible.”
- If you’re on five or more medications, ask for a medication review. Polypharmacy patients are the most likely to have conflicting food rules.

9 Comments
Let’s be real-most people treat their prescriptions like they’re cereal: just dump it in and hope for the best. The fact that 78% of new drugs have food interaction guidelines and yet 68% of seniors don’t even know the rules? That’s not negligence. That’s a public health failure dressed in blue pill bottles. I’ve seen patients on warfarin go from stable INRs to ER visits because they suddenly went vegan. No one warns them. Pharmacists are overworked. Doctors don’t have time. And yet, we act surprised when someone ends up with a GI bleed from ibuprofen on an empty stomach. This isn’t rocket science-it’s basic physiology. Stop treating your meds like candy.
And don’t get me started on grapefruit juice. It’s not a ‘health trend.’ It’s a silent drug assassin. If your doctor didn’t tell you to avoid it, they didn’t do their job. Period.
Also, ‘take with food’ doesn’t mean a single almond. It means a meal. A real one. Not a protein bar you bought at the gas station.
Someone needs to put this on a billboard.
Also, smart pills? Finally. Took long enough.
And yes, I’ve read every study cited here. And no, I’m not exaggerating.
Also, I work in clinical pharmacy. I’ve seen it all.
Also, your ‘I’ve taken it this way for years’ excuse? Doesn’t hold up in a court of law. Or a hospital chart.
I took metformin on an empty stomach for six months and thought I was just ‘sensitive.’ Turns out I was just stupid. The nausea was so bad I’d cry after dinner. Started taking it with my evening meal-suddenly I could eat without feeling like I was going to vomit my organs out. No one told me. Not my doctor. Not the pharmacist. Just a random comment on a forum. I wish I’d found this article six months ago.
You people are so irresponsible. You take your medicine like it’s a snack. You eat junk, drink soda, then swallow your pills like it’s nothing. And then you wonder why you’re sick. It’s not the medicine-it’s YOU. You don’t care about your body. You don’t care about rules. You want convenience. Well, guess what? Your body doesn’t care about your convenience. It’s not a vending machine. You don’t get to press a button and get results. You have to follow the rules. Or suffer. Simple as that.
This was so helpful-and honestly, a relief. I’ve been taking levothyroxine with my morning coffee because I thought ‘empty stomach’ just meant no breakfast yet. Turns out coffee counts too. I’ve been doing it wrong for years. Just switched to taking it at bedtime (after my last snack) and my TSH levels dropped into range within 6 weeks. I’m so glad I read this. Thank you for writing it with such clear examples. I’m printing this out and taping it to my pill organizer. You made something scary feel manageable.
Also, if you’re on multiple meds and feel overwhelmed-you’re not alone. This article is a lifeline.
One thing this doesn’t mention enough: timing between meals and meds matters even more than the food itself. I’m on three meds that all have conflicting food rules. One needs 2 hours before, another 1 hour after, and the third needs fat. I ended up scheduling them around my meals like a military operation. Set alarms. Used a food log app. Took a photo of the label every time I got a refill. It’s annoying, but it works. My doctor was shocked when my lab results improved. I didn’t change the dosage-I changed the timing. Small changes, huge impact.
As someone from India where dietary habits vary widely across regions, I’ve observed that traditional meals often naturally align with medication requirements. For example, many Indian households consume lentils and rice with meals, which provide sufficient bulk and fat to aid absorption of certain drugs. However, the lack of patient education remains universal. A simple visual chart at the pharmacy counter, perhaps with local food examples-like ‘take with dal-chawal’ or ‘avoid with lemon water’-could bridge the gap. Language is not the barrier; clarity is. This article is excellent, but its principles must be localized to be truly effective.
I just had a panic attack reading this. I’ve been taking methotrexate with a granola bar for two years. TWO YEARS. I thought ‘with food’ meant anything that wasn’t pure air. I’ve been throwing up every week. I thought it was ‘just part of it.’ I just called my rheumatologist. I’m going in tomorrow. I’m so mad at myself. But also… thank you. I didn’t know. No one told me. And now I know. I’m going to scream this from the rooftops. I’m printing this and giving it to everyone I know on meds. You saved me from myself.
While the clinical data presented is both compelling and rigorously substantiated, I would respectfully posit that the cultural and socioeconomic dimensions of medication adherence remain underexplored in this discourse. In many households, particularly among low-income populations, the notion of ‘a meal’ as defined by the FDA-250–500 calories-is a luxury. A single banana, a slice of bread, or a cup of tea may constitute ‘food’ in the absence of more substantial options. To prescribe adherence without acknowledging structural barriers to nutrition is, in effect, to blame the patient for systemic failures. A truly comprehensive approach must integrate nutritional support services with pharmaceutical counseling. This article, while informative, risks reinforcing stigma unless contextualized within broader public health equity frameworks.
OMG OMG OMG THIS IS WHY AMERICA IS FALLING APART!!! PEOPLE ARE JUST SWALLOWING PILLS LIKE THEY’RE CANDY!!! NO ONE CARES ABOUT SCIENCE ANYMORE!!! I’VE BEEN TELLING PEOPLE FOR YEARS THAT GRAPEFRUIT JUICE IS A DRUG KILLER!!! AND NOW THE FDA IS MAKING SMART PILLS??? WHO’S NEXT?? ROBOT DOCTORS???!!! I SAW A GUY TAKE IBUPROFEN WITH A COKE AND A DONUT THE OTHER DAY!!! HE WAS SMILING!!! HOW IS THIS EVEN LEGAL???!!! I’M CALLING MY CONGRESSMAN!!! THIS IS A NATIONAL EMERGENCY!!! 🚨💥😭💊🇺🇸