
More than 1 in 25 pregnant women in the U.S. are now taking gabapentin or pregabalin during pregnancy. That’s up from less than 1 in 500 just 20 years ago. These drugs, originally meant for seizures and nerve pain, are now commonly prescribed for chronic back pain, fibromyalgia, anxiety, and even insomnia in pregnant women. But as their use has soared, so have questions: Is it safe for the baby?
What Are Gabapentinoids, and Why Are They Used in Pregnancy?
Gabapentin (Neurontin) and pregabalin (Lyrica) are not traditional painkillers like opioids or NSAIDs. They work by calming overactive nerves, making them useful for conditions that don’t respond well to other treatments. For some pregnant women, this means relief from severe neuropathic pain that hasn’t improved with physical therapy, acupuncture, or even acetaminophen. Others take them for anxiety or restless legs syndrome that disrupts sleep.
What makes them attractive to doctors? Unlike opioids, they don’t cause respiratory depression. Unlike benzodiazepines, they aren’t strongly linked to birth defects. But that doesn’t mean they’re harmless. Both drugs cross the placenta easily. Studies show they reach the fetal bloodstream at levels close to the mother’s. That means the developing baby is exposed for hours, every day, if the mother takes the medication regularly.
Major Birth Defects: The Numbers Don’t Tell the Whole Story
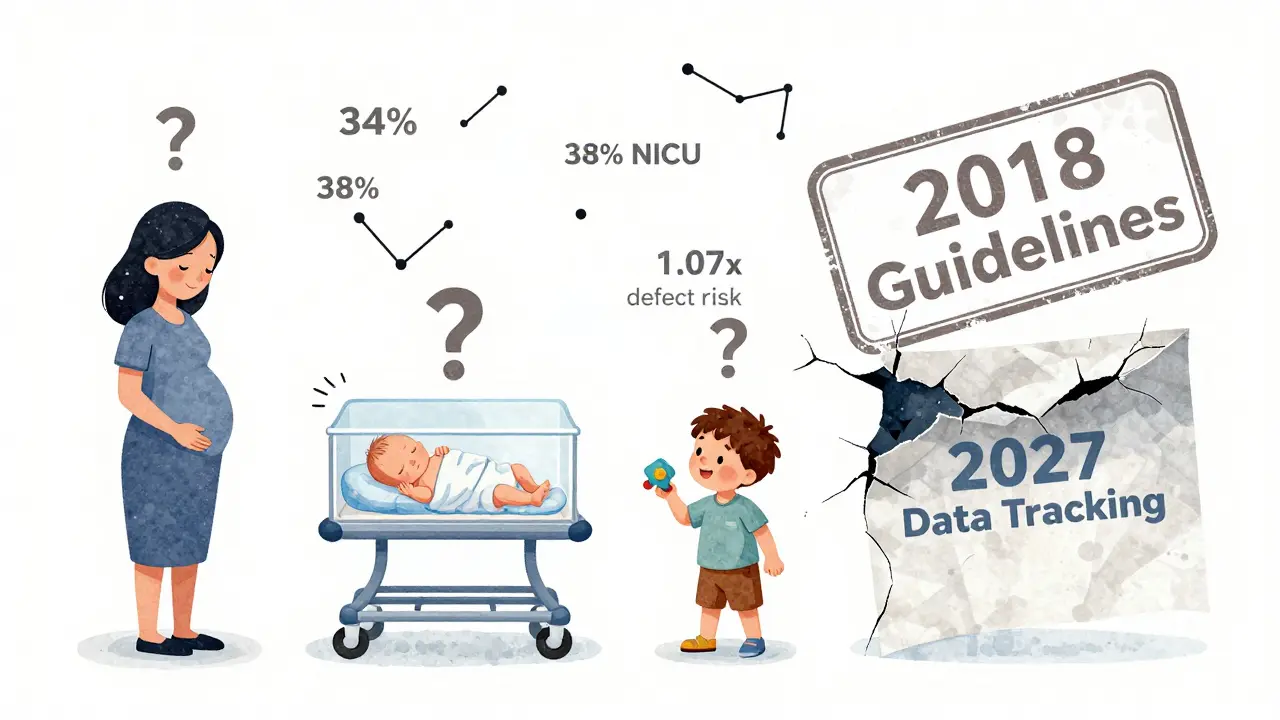
The most reassuring finding from large studies is that gabapentinoids don’t cause a big spike in major birth defects like heart malformations, cleft lip, or spina bifida. The overall risk increase is small - about 1.07 times higher than in unexposed pregnancies. That means if the baseline risk is 3%, it rises to about 3.2%. For comparison, valproic acid, an older seizure drug, carries a 10% to 11% risk of major defects.
But here’s the catch: one specific type of heart defect - conotruncal defects - shows a clearer signal. These involve problems with how the outflow tracts of the heart form. The risk doubles in women who take gabapentin consistently (two or more prescriptions) during early pregnancy. That’s not common, but it’s enough to matter. When you’re expecting a baby, even a 0.8% risk (up from 0.6%) is worth talking about. That’s why doctors now recommend a detailed fetal echocardiogram around 20 weeks if gabapentin has been taken regularly.
Preterm Birth and Low Birth Weight Are Real Concerns
The biggest red flags aren’t birth defects - they’re what happens after birth. Women who take gabapentinoids late in pregnancy are 34% more likely to deliver early. They’re also 22% more likely to have a baby who’s small for gestational age. These aren’t minor issues. Preterm babies face higher risks of breathing problems, feeding difficulties, infections, and long-term developmental delays.
Why does this happen? It’s not fully understood. One theory is that gabapentin affects hormones involved in labor timing. Another is that it interferes with placental function. Either way, the data is consistent across multiple studies. In one study of nearly 1.8 million pregnancies, the rate of preterm birth jumped from 9% in unexposed women to 12% in those taking gabapentin.

Neonatal Adaptation Syndrome: What Happens After Delivery?
Think of this like a baby going through withdrawal - but not from opioids. It’s called neonatal adaptation syndrome. About 38% of babies exposed to gabapentin until delivery end up in the NICU, compared to just 3% of babies not exposed. Why? These infants often show symptoms within hours or days after birth: jitteriness, high-pitched crying, trouble feeding, rapid breathing, or even seizures in rare cases.
It’s not addiction in the adult sense. The baby’s nervous system has adapted to the drug’s presence and now has to readjust on its own. The good news? Most symptoms resolve within a few days to two weeks with supportive care - extra feeding, swaddling, quiet environment. But the bad news? It’s unpredictable. One baby might be fine; another might need weeks of monitoring. And there’s no reliable way to know which one it will be.
What About Pregabalin vs. Gabapentin?
Pregabalin is stronger, faster-acting, and more likely to be prescribed for anxiety. But it’s also more potent in crossing the placenta. Animal studies show pregabalin causes more significant developmental changes at lower doses than gabapentin. In 2022, the European Medicines Agency warned that pregabalin should be avoided in pregnancy unless absolutely necessary. The FDA hasn’t changed its labeling yet, but many U.S. doctors are now steering clear of pregabalin in pregnant patients altogether.
Gabapentin is still used more often - partly because it’s cheaper and available as a generic. But it’s not safer. The same risks apply. The key difference? Pregabalin’s effects appear more pronounced, and its decline in use during pregnancy is already happening in Europe. In the U.S., it’s still prescribed, but fewer doctors are comfortable doing so.
When Might Gabapentin Still Be the Right Choice?
There are cases where the risks of not taking the drug outweigh the risks of taking it. Think of a woman with severe, disabling neuropathic pain from diabetic nerve damage or post-surgical nerve injury. If she can’t walk, can’t sleep, or is on high-dose opioids, gabapentin might be the only option that gives her real relief - and improves her ability to care for herself and her baby.
Experts agree: don’t stop gabapentin cold turkey if you’re already taking it. Sudden withdrawal can trigger seizures or rebound pain, which is dangerous for both mother and fetus. If you’re planning pregnancy, talk to your doctor at least 3 to 6 months ahead. Can your pain be managed with physical therapy, TENS units, or non-drug options? Are there safer alternatives like duloxetine (Cymbalta), which has better pregnancy safety data?
For women already pregnant and on gabapentin, the goal isn’t always to stop - it’s to use the lowest effective dose for the shortest time. Avoiding use after 32 weeks can significantly reduce NICU admission risk. If you’re taking it for anxiety or insomnia, your doctor might recommend tapering off in the third trimester.
What Should You Do If You’re Taking Gabapentinoids and Pregnant?
Don’t panic. Don’t stop on your own. Do these three things:
- Talk to your OB-GYN and prescribing doctor together. Bring your full medication list. Ask: "Is this still necessary? Can we lower the dose? Are there alternatives?"
- Request a detailed fetal anatomy scan and echocardiogram. Even if you’ve only taken it once, mention it. These tests can catch structural issues early.
- Plan for postpartum monitoring. Tell your pediatrician you took gabapentin during pregnancy. They should watch for jitteriness, feeding problems, or breathing issues in the first 72 hours.
Also, keep a log: what dose, when you took it, how you felt. This helps your care team make better decisions.
The Bigger Picture: Why Is This Happening?
Doctors aren’t ignoring the risks. The problem is that for many patients, there are few good options. Opioids are dangerous. NSAIDs are risky after 20 weeks. Antidepressants like SSRIs carry their own fetal concerns. Gabapentinoids filled a gap - and they were marketed as safe.
Now, we know better. But changing prescribing habits takes time. A 2023 survey found nearly half of U.S. hospitals still use outdated guidelines from before 2018. The FDA just announced a new requirement: all manufacturers must track 5,000 pregnancy outcomes by 2027. That’s a step forward. But it’s reactive - not preventive.
Meanwhile, research is underway to see if children exposed to gabapentinoids have long-term learning, motor, or behavioral differences. The first results from a major NIH study tracking 1,200 children are expected in late 2025. Until then, we’re making decisions with incomplete data.
Bottom Line: It’s Not Black and White
Gabapentinoids aren’t the next thalidomide. They don’t cause massive waves of birth defects. But they’re not harmless either. The risks are subtle, delayed, and often missed - preterm birth, NICU stays, subtle heart issues, neonatal distress.
If you’re pregnant and taking gabapentin or pregabalin, your best move is to have an honest, detailed conversation with your care team. Ask: "Is this still needed? Can we try something else? What happens if we stop? What happens if we keep going?"
There’s no one-size-fits-all answer. But the goal is simple: protect the baby without sacrificing the mother’s health. That balance is possible - but only if you’re informed, involved, and supported.






15 Comments
Gabapentin was prescribed to me for anxiety in my third trimester and I was terrified. But my pain was so bad I couldn’t sleep or sit down. We tapered slowly after 32 weeks and my baby had a rough 48 hours but pulled through. He’s now a healthy 2-year-old. Don’t panic, but don’t ignore it either.
I had a friend whose baby went to NICU for 10 days after she took gabapentin till delivery. No major defects, just jittery, screaming, couldn’t latch. They didn’t warn her until after. This needs to be standard info at every OB appointment.
Just read the FDA’s 2024 safety update - pregabalin’s placental transfer rate is 1.8x higher than gabapentin. That’s not even up for debate anymore. If you’re on pregabalin and pregnant, ask for a switch. Now.
My OB didn’t even mention gabapentin risks until I brought it up myself. I was on it for fibromyalgia and thought it was safe because it’s not an opioid. Turns out, doctors are still relying on outdated guidelines. We need better education - stat.
My sister took gabapentin for RLS and had a preterm baby at 34 weeks. She didn’t know the risks. Now she’s a mom who advocates for better prenatal med counseling. If you’re on this stuff, talk to someone. Don’t wait.
Here in India, gabapentin is sold over the counter like candy. Pregnant women take it for insomnia without a clue. We need public health campaigns, not just doctor-to-patient talk. This is a silent epidemic.
It’s funny how we treat pregnancy like a disease to be managed with pills instead of a natural process to be supported. We’ve got yoga, acupuncture, sleep hygiene, nutritional support - but we default to the pill because it’s faster. Gabapentin isn’t evil, but our system is lazy.
Let’s be real - gabapentinoids are the pharmaceutical industry’s Band-Aid on a bullet wound. We’re replacing opioids with something ‘safer’ but still toxic to developing nervous systems. And we call it progress? 🤦♂️
As a neonatologist, I’ve seen 17 cases of neonatal adaptation syndrome linked to gabapentin in the last 3 years. Every single one was preventable. The key is early discussion, dose reduction after 32 weeks, and neonatal monitoring. It’s not rocket science - it’s standard of care.
Why are we even allowing this? The FDA is asleep at the wheel. In Europe, pregabalin is banned in pregnancy. In the U.S., we let Big Pharma dictate safety. This is negligence. Someone needs to be held accountable.
Why do American women take so many drugs during pregnancy? In my country, we use herbs, rest, and tradition. No pills. No problems. This is what happens when you trust chemists over culture.
I took gabapentin for 8 months pregnant and my kid is perfect. So why are you all freaking out? It’s not a poison. You’re just scared of modern medicine. Stop fearmongering.
How is this even a debate? The data is clear. The risk is statistically significant. If you’re not advocating for immediate cessation in early pregnancy, you’re not doing your due diligence as a clinician.
My OB said ‘it’s fine’ until I showed her the 2023 JAMA study. Then she apologized and switched me to duloxetine. Took a week to adjust but my anxiety is better and my baby’s heart looks perfect on echo. Knowledge is power.
According to the 2024 cohort study published in Obstetrics & Gynecology, the adjusted odds ratio for preterm birth among women exposed to gabapentin in the third trimester was 1.34 (95% CI: 1.19–1.51). The effect size is clinically meaningful and warrants immediate intervention protocols in prenatal care.