What You Need to Know About Bisphosphonates and Jaw Problems
If you're taking a bisphosphonate for osteoporosis, you’ve probably heard whispers about jaw necrosis. Maybe a friend had a tooth pulled and then developed an open sore that wouldn’t heal. Or your dentist paused a cleaning because they’re "afraid" of something called MRONJ. The truth? For most people on these meds, the risk is so low it’s almost theoretical. But when it does happen, it’s serious. And that’s why so many patients feel stuck between two fears: breaking a hip from osteoporosis, or losing part of their jaw from the medicine meant to prevent it.
Let’s cut through the noise. Bisphosphonates - drugs like alendronate (Fosamax), risedronate (Actonel), and ibandronate (Boniva) - have been used for over 25 years to stop bones from crumbling. They work by shutting down the cells that break down bone (osteoclasts). That’s exactly what you want when your bones are thinning. Studies show they reduce hip fractures by up to 51% and spine fractures by nearly half. That’s not small. That’s life-changing. But every medicine has a shadow side. For bisphosphonates, that shadow is medication-related osteonecrosis of the jaw (MRONJ).
What Exactly Is MRONJ?
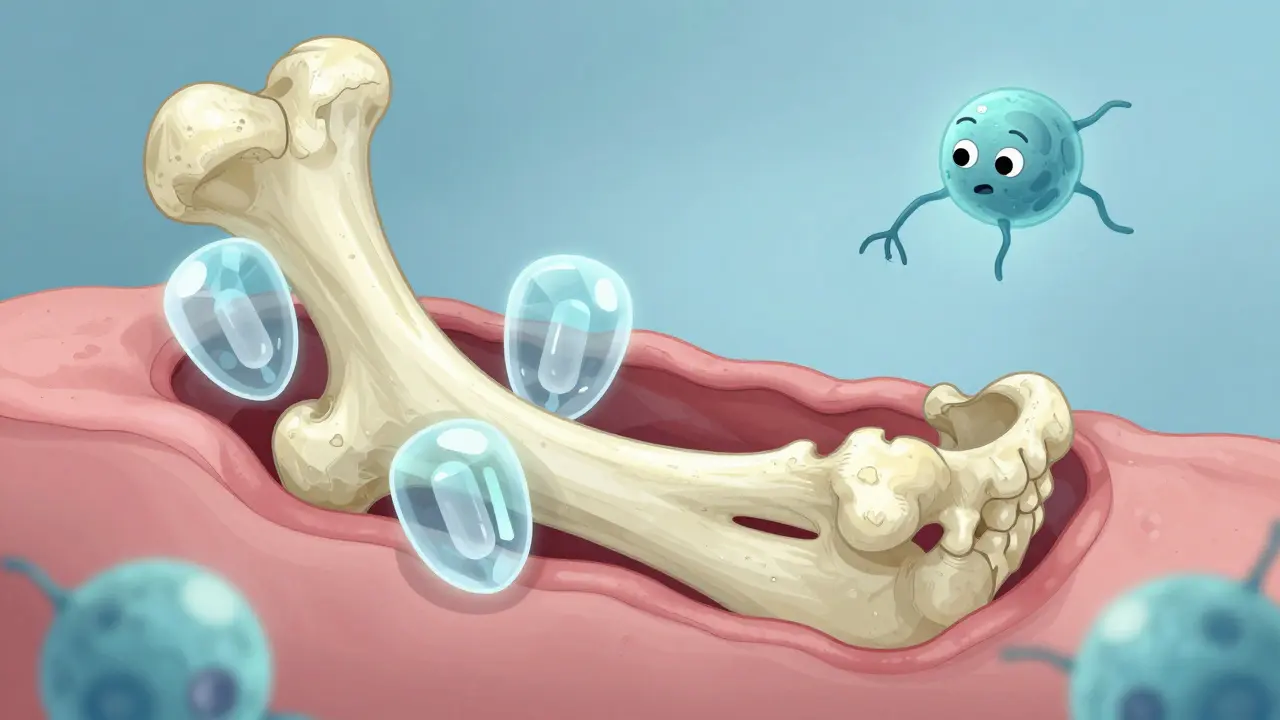
MRONJ isn’t cancer. It’s not infection in the usual sense. It’s a failure of the jawbone to heal. When the bone becomes exposed through the gum tissue and stays exposed for more than eight weeks, that’s the diagnosis. It usually happens after a tooth extraction, but sometimes it starts with a loose tooth or even just gum irritation. The bone doesn’t die from lack of blood - it just stops repairing itself. That’s because bisphosphonates lock onto bone tissue and stay there for years, even decades. They’re like a permanent shield against bone loss… but they also block the natural cleanup crew that rebuilds bone after injury.
The jaw is uniquely vulnerable. Unlike your thigh or hip bone, the jaw is constantly under pressure from chewing, has thin gum tissue, and is full of bacteria. A small cut from a tooth extraction doesn’t heal the same way it would elsewhere. When bisphosphonates are in the system, that cut can turn into an open wound that refuses to close.
How Common Is This Really?
Here’s the key number: for someone taking oral bisphosphonates like alendronate for osteoporosis, the risk of MRONJ is about 0.7 in 100,000 per year. That’s less than one case per 140,000 people annually. To put that in perspective, you’re more likely to be struck by lightning in a given year than develop MRONJ on oral bisphosphonates.
Compare that to cancer patients getting high-dose IV bisphosphonates - their risk is 100 to 1,000 times higher. That’s because they’re getting much stronger doses, often monthly, to fight tumors in bone. But for osteoporosis? You’re getting a tiny fraction of that. A typical alendronate pill is 70mg once a week. A cancer patient gets 4mg of zoledronic acid every three weeks - that’s over 100 times more potent per dose.
A 2011 study of 260,000 osteoporosis patients found no increased risk of jaw necrosis in those taking oral bisphosphonates compared to those who didn’t. In fact, the odds were slightly lower. That’s not a typo. The data doesn’t support the fear.
But What About IV Drugs?
It’s a different story with intravenous bisphosphonates like zoledronic acid (Reclast). These are given once a year for osteoporosis, and the dose is higher than oral versions. The risk jumps to about 1 in 100,000 per year - still very low, but not negligible. A 2024 study in Nature Communications tracked over 600 patients and found that if you stop IV bisphosphonates for more than a year, your risk of MRONJ drops by 82%. But here’s the catch: stopping also increases your fracture risk by 28%. That’s a real trade-off.
Denosumab (Prolia), another osteoporosis drug, carries a slightly higher risk than oral bisphosphonates - about 1.7 to 2.5 times higher. But even then, the absolute risk remains under 1 in 10,000 per year. And like bisphosphonates, it works by stopping bone breakdown. The difference? It’s a monoclonal antibody, not a bone-binding chemical. It leaves your system faster, but it also needs to be injected every six months. Miss a dose, and your bone protection vanishes.

Who’s at Highest Risk?
Most cases of MRONJ happen after dental surgery - especially tooth extractions. About 63% of cases in osteoporosis patients follow a tooth removal. The median time from surgery to diagnosis? Two years. That’s not immediate. It’s slow. And it’s not random. The biggest risk factor isn’t the drug - it’s your dental health before you start.
If you already have gum disease, infected teeth, or ill-fitting dentures, you’re already at risk for jaw problems. Adding a bisphosphonate doesn’t create the problem - it just makes healing harder. That’s why experts say: get your mouth in good shape before you start treatment. Clean teeth. No loose teeth. No active infections. Fill cavities. Get dentures adjusted. Do this within 30 days of starting an IV bisphosphonate.
Smokers, diabetics, and people on steroids have higher risk too. Poor blood sugar control slows healing. Smoking kills blood flow. Steroids suppress immune response. All of these make jaw healing harder - with or without bisphosphonates.
What Should You Do Before a Dental Procedure?
Don’t panic. Don’t stop your medicine unless your doctor says so. Most dentists and oral surgeons know how to handle this now. For simple cleanings and fillings? No changes needed. Your bisphosphonate isn’t a barrier.
For extractions or implants? Talk to both your doctor and your dentist. If you’ve been on IV bisphosphonates for more than three years, some doctors may suggest a drug holiday - pausing the IV for 3 to 6 months before and after surgery. But for oral bisphosphonates? The guidelines don’t recommend stopping. The fracture risk outweighs the tiny MRONJ risk.
And here’s something most people don’t know: if you’ve been on bisphosphonates for over five years, your bone still holds the drug. Even if you stopped five years ago, your jawbone is still affected. That’s why your dentist needs to know your full history - not just what you’re taking now.
Signs You Might Have MRONJ
Early MRONJ often has no pain. That’s why it’s missed. Stage 1: exposed bone in the mouth, no infection, no symptoms. Stage 2: bone exposed, with pain, swelling, or pus. Stage 3: bone breaks through the jaw, or a hole opens into the face.
If you notice any of these after a dental procedure - especially if it’s been more than 8 weeks and the area hasn’t healed - tell your dentist immediately. Don’t wait. Early treatment (antibiotics, mouth rinses, gentle cleaning) can stop it from getting worse. Surgery is usually only needed if it’s advanced.

Why Do So Many People Fear This?
Because the stories are scary. One woman on a patient forum spent 18 months with an open jaw wound after a cleaning. Another man had multiple implants and never had an issue. Both are real. But the media and internet amplify the worst cases. The truth? Out of 1,247 patient comments on dental forums, only 2.3% reported actual MRONJ. Yet 87% said they were anxious before any dental work.
Many dentists, afraid of lawsuits, refuse to pull teeth on bisphosphonate users. That’s not evidence-based. It’s fear-driven. The American Dental Association and the American Association of Oral and Maxillofacial Surgeons both say: treat the patient. Don’t avoid care. The risk of a broken hip is far greater than the risk of jaw necrosis.
Alternatives to Bisphosphonates
If you’re terrified of MRONJ, there are other options. Denosumab is one. Romosozumab (Evenity) is newer - it builds bone instead of just slowing loss. But it’s expensive, given as monthly injections for just one year, and requires follow-up with another drug. It’s not for everyone.
The bottom line? No alternative matches the long-term fracture protection of bisphosphonates. A 11-year study of alendronate users showed a 55% reduction in hip fractures. That’s unmatched. And for most people, the trade-off is worth it.
What’s Next?
Doctors are moving toward personalized treatment. Soon, we may test your bone turnover markers - like NTX in your urine - to see how active your bone is. If it’s low, you might be at higher risk for MRONJ. Then, instead of giving you five years of alendronate, your doctor might stop after two or three. Or switch you to a different drug.
For now, the best advice is simple: if you’re on bisphosphonates, keep your mouth healthy. Brush, floss, see your dentist every six months. Don’t delay needed care. Don’t stop your medicine without talking to your doctor. And remember: the chance you’ll break a hip without this drug is hundreds of times higher than the chance you’ll develop jaw necrosis with it.






9 Comments