SGLT2 Inhibitor Fluid Loss Calculator
Fluid Needs Calculator
SGLT2 inhibitors cause increased urine production as they remove glucose from the bloodstream. This can lead to dehydration, dizziness, and low blood pressure. Calculate your daily fluid requirements to stay safe while on these medications.
Your Inputs
Your Results
Estimated fluid loss: 0.0 L
Recommended daily fluid intake: 0.0 L
Tips for staying safe:
- Drink water regularly throughout the day
- Monitor for signs of dehydration like dry mouth or dizziness
- Avoid standing up too quickly
When you start taking an SGLT2 inhibitor for type 2 diabetes, you might not expect to feel dizzy or unusually thirsty. But these aren’t rare side effects-they’re direct results of how the drug works. SGLT2 inhibitors like empagliflozin (Jardiance®), dapagliflozin (Farxiga®), and canagliflozin (Invokana®) don’t just lower blood sugar. They turn your kidneys into natural diuretics. And that’s where the real trade-off lies: big benefits for your heart and kidneys, but real risks of dehydration, dizziness, and low blood pressure.
How SGLT2 Inhibitors Work (And Why They Cause Diuresis)
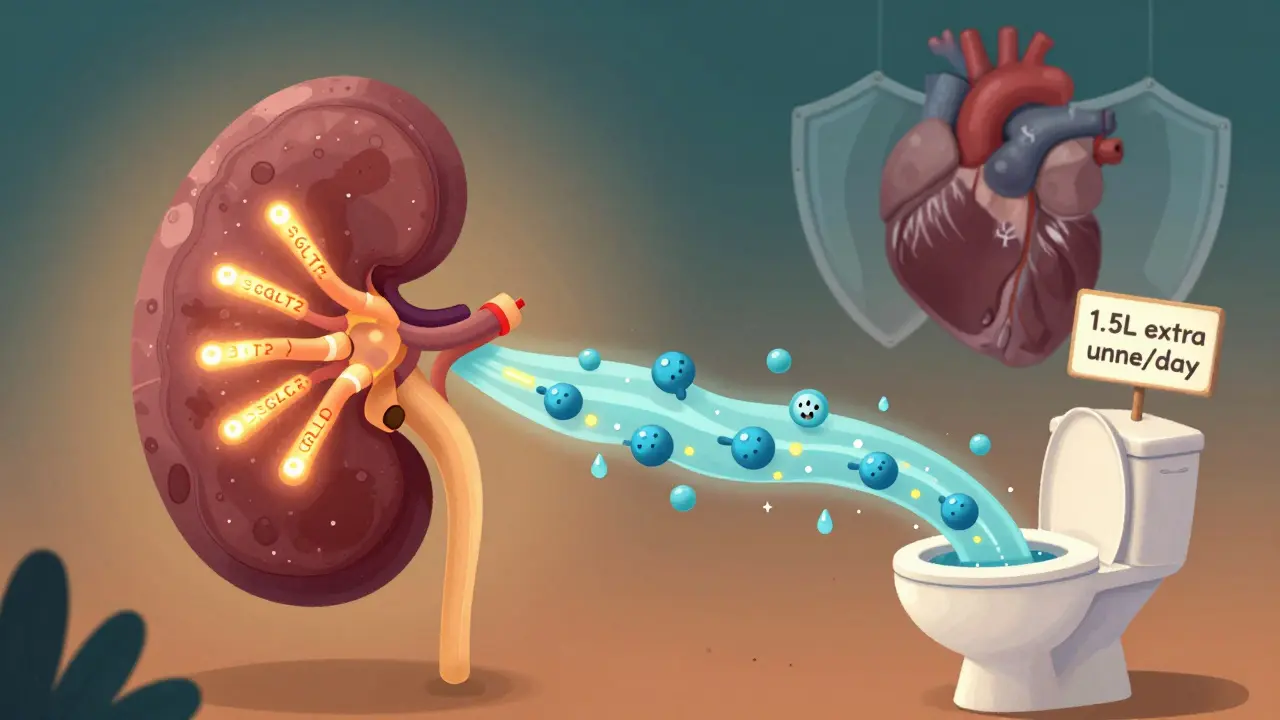
These drugs block a protein in your kidneys called SGLT2. Normally, this protein grabs glucose from your blood and reabsorbs it back into your body. But SGLT2 inhibitors stop that. Instead, glucose gets flushed out in your urine-about 70 to 100 grams per day. That’s roughly 300 calories lost daily, which is why many people lose weight on these drugs.
But here’s the catch: glucose doesn’t leave alone. It drags sodium and water with it. For every gram of glucose excreted, about 3 milliliters of water follows. That’s why people on these drugs often pee more-sometimes 1 to 1.5 liters extra per day in the first week. This isn’t just a side effect. It’s the main mechanism behind their heart and kidney benefits. Less fluid in the blood vessels means lower pressure on the heart and less strain on the kidneys.
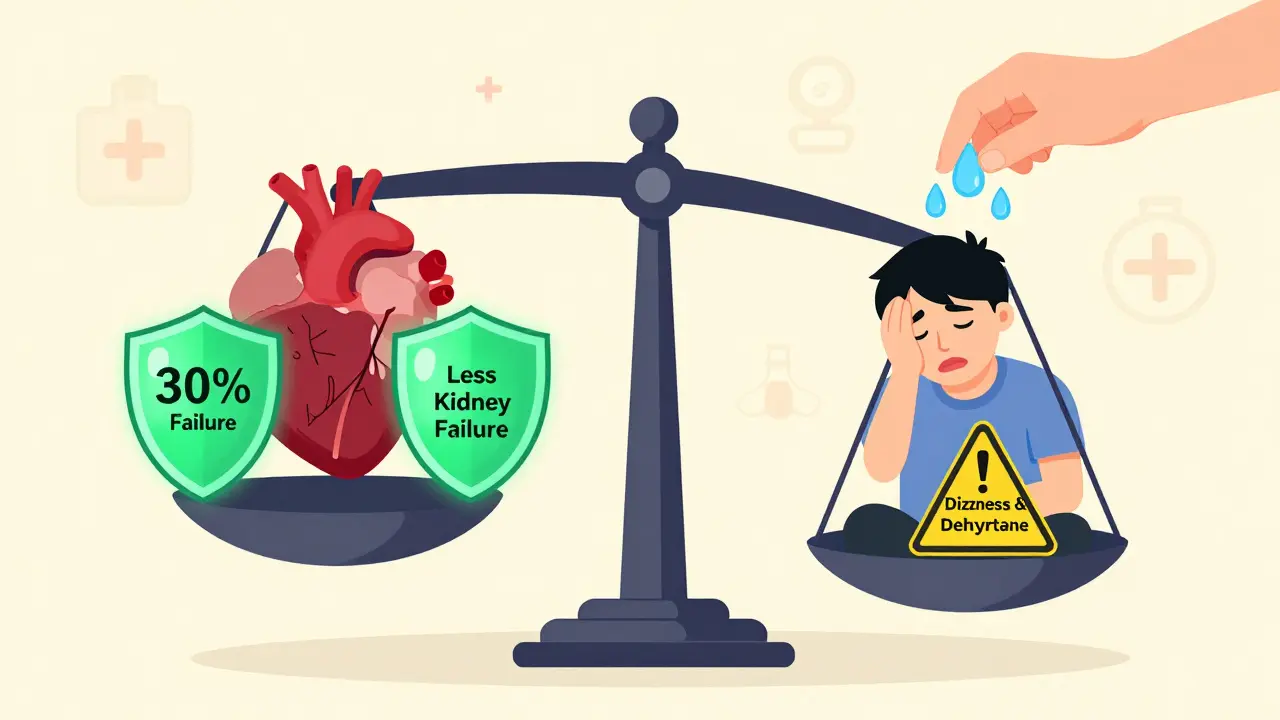
Studies show that within two weeks, systolic blood pressure drops by 4 to 6 mmHg on average. That’s similar to the effect of a low-dose diuretic. But unlike traditional diuretics, SGLT2 inhibitors don’t just pull water out-they also reduce arterial stiffness and improve blood vessel function. That’s why they lower heart failure risk by up to 20% in trials like DAPA-HF and EMPEROR-Reduced.
Dehydration: More Common Than You Think
Dehydration from SGLT2 inhibitors isn’t a myth. It’s a documented risk. In clinical trials, 1.3% to 2.8% of users experienced volume depletion symptoms like dry mouth, fatigue, or low blood pressure. That might sound low, but it’s nearly triple the rate of placebo groups. The risk jumps sharply in certain groups:
- People over 65
- Those with kidney function below 60 mL/min (eGFR)
- Patients already on diuretics or blood pressure meds like ACE inhibitors
- Anyone in hot weather or who exercises without drinking enough
A study in the New England Journal of Medicine found that patients with baseline systolic blood pressure under 120 mmHg had over three times the risk of symptomatic low blood pressure. Older adults are especially vulnerable because their thirst sense fades with age. One patient in a Reddit forum wrote: "I started Jardiance and felt like I was constantly thirsty, but my mouth stayed dry. I didn’t realize I was dehydrating until I nearly passed out standing up."
Hospitalization rates for volume depletion are higher in this group-0.8% on SGLT2 inhibitors versus 0.4% on placebo. That’s why doctors now recommend checking your hydration status before starting. If you’re already dehydrated from illness, heat, or poor fluid intake, this drug can push you over the edge.
Dizziness: A Signal, Not Just an Annoyance
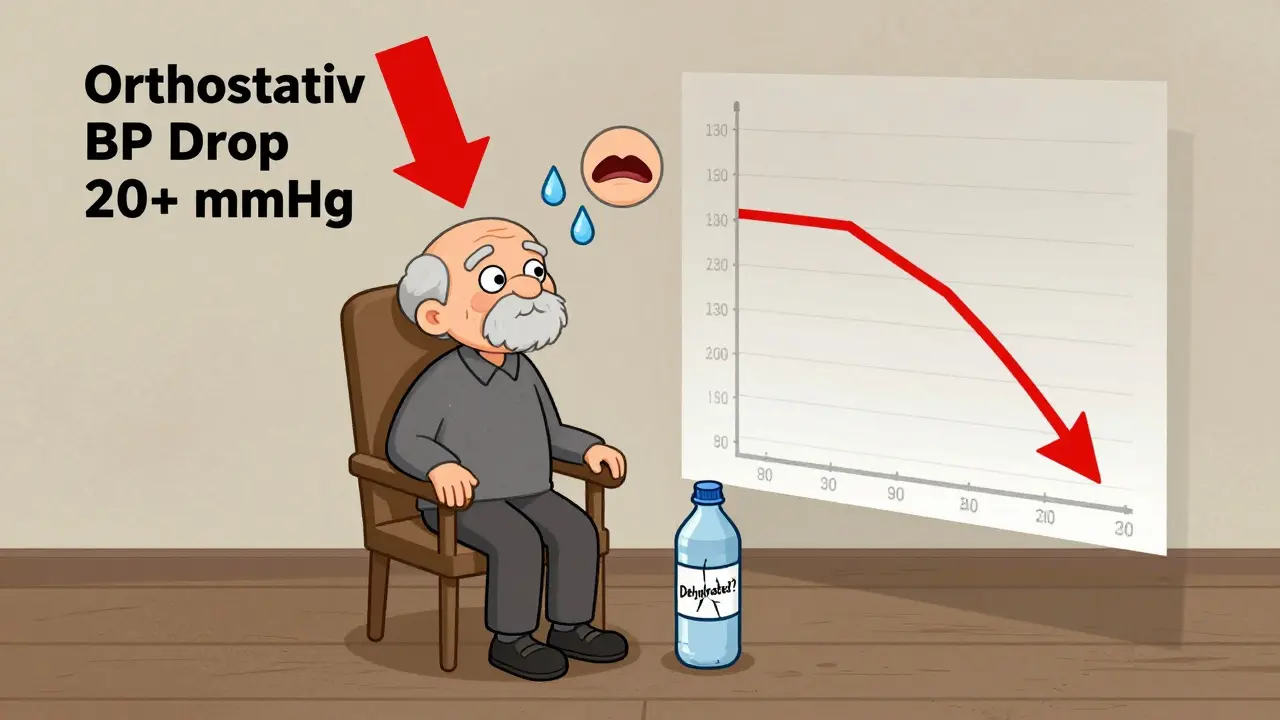
Dizziness is one of the most reported side effects. In trials, 3.5% to 5.8% of users felt lightheaded-compared to 2.5% to 3.2% on placebo. But here’s what most people don’t realize: dizziness from SGLT2 inhibitors isn’t random. It’s almost always linked to orthostatic hypotension-your blood pressure dropping too fast when you stand up.
Studies show that 63% of dizziness cases happen when patients stand up, and their systolic pressure falls by more than 20 mmHg. This usually occurs within the first 4 weeks, right when fluid loss peaks. The risk is highest if you’re over 75, on multiple blood pressure meds, or already have low blood pressure.
Canagliflozin has the highest reported dizziness rate-6.3 cases per 1,000 patient-years-likely because it’s the most potent at causing sodium excretion. Dapagliflozin and empagliflozin are slightly lower. But even the "milder" ones still cause dizziness in nearly 1 in 20 users.
On Drugs.com, over 38% of empagliflozin users reported dizziness. Most described it as mild and temporary. But nearly 30% said it was bad enough to consider stopping. That’s a red flag. Dizziness isn’t just uncomfortable-it’s a fall risk, especially in older adults.
Low Blood Pressure: The Hidden Benefit and Real Danger
Lower blood pressure sounds like a good thing, right? For many, it is. SGLT2 inhibitors reduce systolic pressure by 4-6 mmHg and diastolic by 1-2 mmHg. That’s enough to cut stroke and heart attack risk over time. But in some people, it’s too much.
The real danger isn’t chronic low pressure-it’s sudden drops. When your body hasn’t adjusted to losing 1-1.5 liters of fluid in the first week, standing up can cause a crash. That’s why doctors now check orthostatic blood pressure before and after starting these drugs. If your systolic pressure falls below 90 mmHg when standing, or if you feel faint, the drug may need to be paused or lowered.
Interestingly, the blood pressure drop happens even in people without diabetes. That’s why these drugs are now approved for heart failure regardless of whether someone has diabetes. But it also means non-diabetic patients-often older and on multiple meds-are at higher risk of complications.
Who Should Be Extra Cautious?
Not everyone should start an SGLT2 inhibitor without precautions. Here’s who needs special care:
- Patients over 65: Higher risk of dehydration and dizziness. Start with the lowest dose.
- People with kidney disease (eGFR <60): Reduced fluid clearance means slower adjustment. Monitor closely.
- Those on diuretics, ACE inhibitors, or ARBs: These drugs add to the diuretic effect. Your doctor may need to lower their doses.
- People with low baseline BP (<120 systolic): You’re more likely to drop too low. Consider alternatives.
- Anyone with recent illness, vomiting, or diarrhea: Hold the drug until you’re hydrated again.
Guidelines from the American Diabetes Association and European Society of Cardiology now recommend checking blood pressure and volume status before starting-and again at one week. If you’re dizzy or dry-mouthed, don’t ignore it. Talk to your doctor. You might need to reduce your dose, hold the drug temporarily, or increase fluid intake.
What You Can Do to Stay Safe
These drugs are powerful. And they save lives. But they need smart management. Here’s how to stay safe:
- Drink more water: Add 500-1000 mL (about 2-4 cups) daily, especially in heat or during exercise.
- Check your weight: Weigh yourself weekly. A drop of 1.5-2.5 kg in the first week is normal. More than that? Call your doctor.
- Stand up slowly: If you feel dizzy, sit or lie down. Wait a minute before standing again.
- Watch for signs of dehydration: Dark urine, dry mouth, fatigue, headache, or confusion.
- Don’t skip follow-ups: Your first check-in should be within 7-10 days. That’s when side effects peak.
- Don’t stop on your own: If dizziness is bad, talk to your doctor. They may lower your dose instead of stopping the drug entirely.
Many patients who stick with SGLT2 inhibitors after the first month say the dizziness fades. The benefits-less heart failure, fewer kidney problems, lower A1C, and weight loss-often outweigh the temporary side effects. But you have to get through the first 30 days safely.
When to Call Your Doctor
Call your doctor immediately if you experience:
- Feeling faint or passing out
- Extreme thirst with no relief
- Dark urine or not peeing for 12+ hours
- Confusion, rapid heartbeat, or chest pain
- Significant weight loss (over 3 kg in a week)
These aren’t normal. They could signal severe dehydration or dangerously low blood pressure. Don’t wait. Get help.
Can SGLT2 inhibitors cause kidney damage?
No, they protect the kidneys. SGLT2 inhibitors reduce pressure inside the kidney’s filtering units (glomeruli), slowing decline in kidney function. Studies show they cut the risk of kidney failure by 30-50% in people with type 2 diabetes and chronic kidney disease. But they can worsen dehydration in those with very poor kidney function (eGFR below 30), so they’re not used in advanced stages.
Is dizziness from SGLT2 inhibitors permanent?
No. In most cases, dizziness fades after 2-4 weeks as your body adjusts to lower fluid volume. If it persists beyond 6 weeks, your doctor may lower your dose or check for other causes like low sodium or anemia. It’s rarely permanent.
Do I need to stop SGLT2 inhibitors before surgery?
Yes. Most guidelines recommend stopping SGLT2 inhibitors 3-4 days before surgery. The risk of dehydration and low blood pressure increases during fasting and anesthesia. Your doctor will tell you when to restart it after recovery.
Can I take SGLT2 inhibitors if I have low blood pressure?
It depends. If your systolic pressure is below 110 mmHg at rest, your doctor may avoid starting one. If you’re on multiple blood pressure meds, they’ll likely reduce those first. But if your low BP is well-controlled and you have heart failure, the benefits may still outweigh the risks-especially with careful monitoring.
Are generic SGLT2 inhibitors as safe as brand names?
Yes. Generic versions of empagliflozin and dapagliflozin have been available since 2023 and are bioequivalent to brand names. The active ingredient is the same. Side effect profiles are identical. The only difference is cost.
Final Thoughts
SGLT2 inhibitors are one of the most important advances in diabetes care in the last decade. They don’t just manage blood sugar-they protect your heart and kidneys. But they’re not harmless. The same mechanism that saves lives can also make you dizzy or dehydrated. The key is awareness. Know your risks. Drink water. Watch for warning signs. And don’t be afraid to speak up if something feels off. You’re not overreacting. You’re being smart.


13 Comments