Bleeding Risk Calculator for Blood Thinners
This tool calculates your HAS-BLED score based on factors from the American Thrombosis Association guidelines. A score of 3 or higher indicates increased risk requiring extra precautions.
Input Your Risk Factors
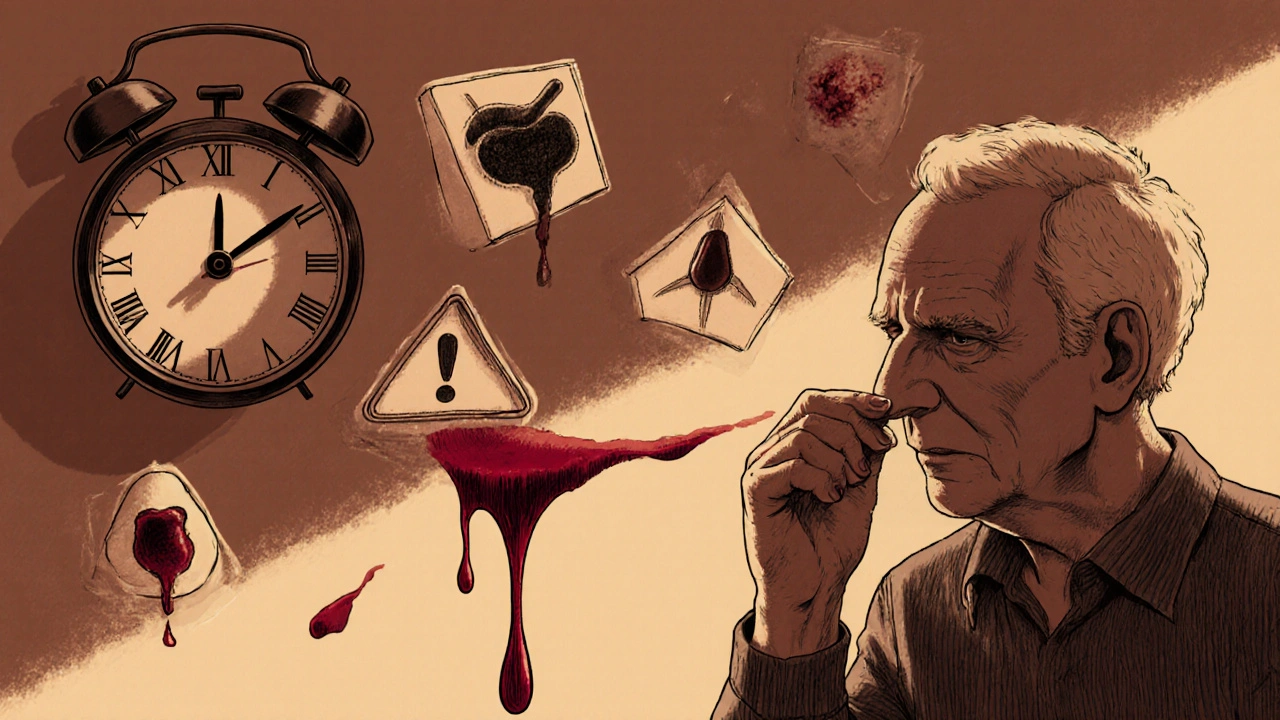
Emergency Response: If you're experiencing any of these symptoms:
• Nosebleeds lasting more than 10 minutes
• Black, tarry stools
• Coughing or vomiting blood
• Severe headache or confusion
• Dizziness or fainting
Go to the emergency room immediately.
When you're prescribed a blood thinner-whether it's warfarin, apixaban, rivaroxaban, or another anticoagulant-you're told it’s to prevent strokes or clots. But few patients are fully prepared for the flip side: severe bleeding. It doesn’t always come with a siren. Sometimes it starts as a nosebleed that won’t stop. Or dark stools. Or unexplained bruising. And if you don’t recognize it fast enough, it can turn life-threatening in hours.
Why Blood Thinners Cause Severe Bleeding
Blood thinners don’t actually thin your blood. They slow down the clotting process. That’s how they prevent dangerous clots in your heart or brain. But that same mechanism means even a small cut or internal injury can lead to serious bleeding. The risk isn’t theoretical-it’s documented.According to the NHS and Mayo Clinic, about 3.1% of patients on direct oral anticoagulants (DOACs) experience a bleeding event in the first year. And here’s the catch: more than half of those cases happen in people taking low-dose versions. That’s not a mistake. It’s a pattern. Even “safe” doses carry risk, especially early on.
The American Heart Association found that the first 90 days are the most dangerous. Why? Your body is adjusting. Your kidneys and liver are processing the drug. And if you have other risk factors-like being over 75, having kidney problems, or taking aspirin or NSAIDs on top of your blood thinner-your risk jumps dramatically. One study showed that having two or more risk factors increases your chance of major bleeding to 6.5% per year.
Recognizing the Signs Before It’s Too Late
Most people don’t realize they’re bleeding until it’s advanced. That’s because internal bleeding doesn’t always hurt. It doesn’t always bleed out. It just silently drains your body of oxygen.Here are the 12 red flags that require immediate medical attention:
- Nosebleeds lasting more than 10 minutes
- Red or brown urine
- Black, tarry, or bloody stools
- Unexplained large bruises
- Coughing or vomiting blood
- Severe headache or confusion
- Dizziness or fainting
- Sudden weakness or numbness
- Blurred or double vision
- Unusually heavy menstrual bleeding
- Joint swelling or pain after minor injury
- Bleeding from a minor cut that won’t stop
These aren’t just “maybe” signs. They’re clear indicators your body is losing blood faster than it can replace it. A study in JAMA Internal Medicine found that patients who received clear, written instructions about these symptoms were 34% less likely to delay going to the ER. That’s the difference between a quick transfusion and a stroke.
Who’s at Highest Risk-and Why
Not everyone on blood thinners bleeds. But some people are far more vulnerable.Age is a major factor. People over 80 have more than three times the bleeding risk of those under 60. Why? Kidney function declines. Liver metabolism slows. Medications build up. A Swedish study showed major bleeding rates jump from 1.25 per 100 treatment-years in younger adults to 4.33 in those over 80.
Renal impairment is another silent killer. If your kidneys aren’t filtering the drug properly, levels stay too high. The CHEST guidelines say kidney disease triples your bleeding risk. That’s why doctors check creatinine clearance before prescribing DOACs. Rivaroxaban, for example, is reduced from 20 mg to 15 mg daily if your creatinine clearance is between 15 and 50 mL/min.
And then there’s the combo effect. Taking aspirin, ibuprofen, or even certain herbal supplements like ginkgo or fish oil with your anticoagulant doubles your bleeding risk. The New England Journal of Medicine confirmed this in 2014. Many patients don’t realize these over-the-counter items are dangerous when paired with blood thinners.
Which Blood Thinners Carry the Highest Risk?
Not all anticoagulants are equal when it comes to bleeding. The data shows clear differences.Warfarin has been around for decades. It works, but it’s unpredictable. You need frequent INR blood tests to make sure your level is in the narrow 2.0-3.0 range. Miss a test, and you could be over-anticoagulated without knowing it.
DOACs like apixaban, rivaroxaban, dabigatran, and edoxaban were designed to be safer. And in many ways, they are. The ARISTOTLE trial showed apixaban had a 2.13% annual major bleeding rate compared to warfarin’s 3.09%. That’s a 31% reduction.
But here’s the twist: apixaban isn’t always the safest for everyone. For patients with a history of gastrointestinal bleeding, apixaban cuts the risk of recurrence by 31% compared to rivaroxaban. But for others, the difference is smaller. And all DOACs carry a high risk in the first three months-60.8% of bleeding events happen then.
And don’t assume “low dose” means “safe.” A 2024 study found that 58% of bleeding events occurred in patients on low-dose DOACs. Why? Because those patients are often older, sicker, or have kidney issues-and the dose isn’t adjusted enough to match their metabolism.
What Happens in the ER: Emergency Response Steps
If you’re bleeding severely, time is everything. Emergency teams have protocols, but they need your help to act fast.First, stop taking your medication. Don’t wait for instructions. Just stop. Bring your pill bottles with you-every one. The ER staff needs to know exactly what you’re on and what dose.
Second, be ready to answer: When did the bleeding start? What symptoms did you notice? Have you had bleeding before? Have you had surgery or trauma recently? These answers determine how aggressively they treat you.
For warfarin, they’ll give you vitamin K and possibly fresh frozen plasma to reverse the effect. For DOACs, it’s more complex.
- If you’re on dabigatran (Pradaxa), they’ll use idarucizumab. One vial costs $3,500, but it works in minutes.
- If you’re on rivaroxaban, apixaban, or edoxaban, they’ll use andexanet alfa. It costs $12,500 per dose.
These drugs are expensive. Many hospitals don’t keep them on hand. That’s why knowing your medication and having a plan matters.
And if you’re bleeding internally-like in your brain or gut-the stakes are even higher. A brain bleed has a 15% death rate. A GI bleed can drop your hemoglobin so low you need 4 or more units of blood. That’s why any bleeding that requires hospitalization counts as a “clinically relevant” event-even if it’s not labeled “major.”
What Patients Are Really Experiencing
Real stories show how easy it is to miss the signs.One Reddit user, u/ClotSurvivor2020, noticed black stools for three days after taking apixaban. He thought it was diet. By the time he went to the ER, he’d lost enough blood to need a transfusion. Another patient on rivaroxaban had a nosebleed that lasted 45 minutes. She didn’t go to the hospital until she felt dizzy. She lost nearly 30% of her blood volume.
A 2023 survey by the American Thrombosis Association found that 37% of patients waited over two hours to seek help. Nineteen percent waited more than six. Why? They didn’t think it was serious. Or they were afraid of the cost. Or they thought the bleeding would stop on its own.
That’s the gap between medical advice and real-world behavior. The system gives you a checklist. But if you don’t believe the symptoms are urgent, you’ll wait. And waiting kills.
How to Protect Yourself
You can’t eliminate the risk. But you can control it.- Get a HAS-BLED score at your first appointment. This tool scores your bleeding risk based on age, kidney/liver function, history of bleeding, and other factors. A score of 3 or higher means you need extra precautions.
- Keep a list of all your medications-including vitamins and OTC drugs-and review it with your doctor every 3 months.
- If you’re over 75 or have kidney disease, ask about DOAC level testing. The FDA approved the first point-of-care test in January 2024. It’s not perfect, but it tells you if your drug level is too high.
- Wear a medical alert bracelet that says “ON ANTICOAGULANT.”
- Have a plan. Know the nearest ER. Know your doctor’s after-hours number. Keep your medication bottle in your wallet or phone.
And if you’re ever unsure-go to the ER. Better to be checked and safe than to wait and regret it.
The Bigger Picture: Why This Is Getting Worse
More people are on blood thinners than ever. In 2023, 4.7 million Americans were taking DOACs. That’s up from 2.1 million in 2015. At the same time, the population is aging. One in 10 Americans over 65 is now on a blood thinner. That’s triple the rate from 2010.That means more bleeding events. The Agency for Healthcare Research and Quality reports a 27% increase in anticoagulant-related ER visits from 2018 to 2022. Each major bleed costs an average of $18,500. Brain bleeds? Over $52,000.
And the problem isn’t going away. Without better tools to predict and prevent bleeding, experts project that by 2030, these complications will cause 15-18% of preventable hospitalizations in older adults.
But there’s hope. New drugs like milvexian and asundexian are in trials. They aim to prevent clots without increasing bleeding. Early results show 20-25% fewer bleeds. And a universal reversal agent called Ciraparantag could one day stop bleeding from any anticoagulant-no matter which one you’re on.
For now, though, the best defense is knowledge. Know your meds. Know your risks. Know the signs. And never wait to act when something feels wrong.

13 Comments