
When your panic attack hits like a freight train, and your heart is racing, your chest is tight, and you can’t catch your breath - benzodiazepines can feel like a lifeline. They work fast. In under an hour, they calm the storm in your brain. For many people, that’s the first time they’ve felt relief in months. But here’s the catch: what helps today can hurt you tomorrow.
How Benzodiazepines Actually Work
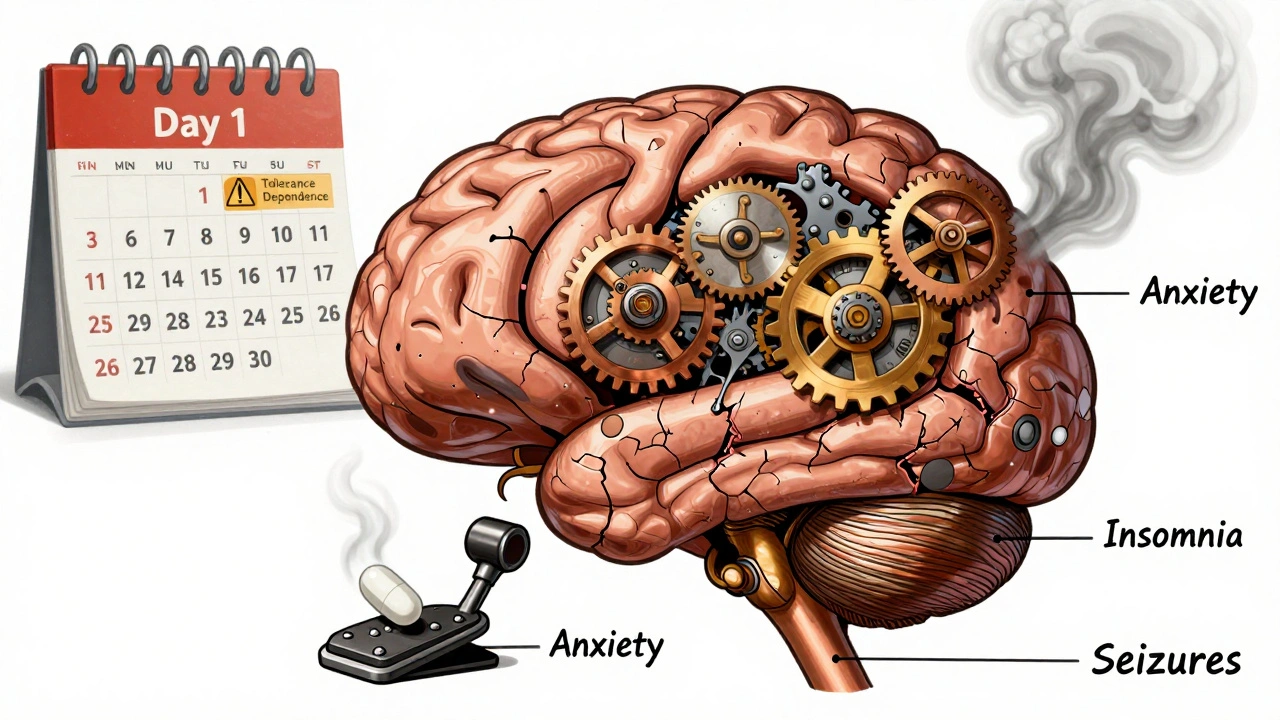
Benzodiazepines don’t just make you sleepy. They target a specific chemical in your brain called GABA. GABA is your brain’s natural brake pedal. It slows down overactive nerve signals that cause anxiety, muscle tension, and seizures. Benzodiazepines, like diazepam, alprazolam, and lorazepam, turn up the volume on GABA. That’s why they’re so effective for sudden panic, muscle spasms, or seizures.
They’re not magic. They’re chemistry. And like any strong chemical, they come with trade-offs. The same mechanism that quiets panic also slows your reflexes, clouds your memory, and makes you drowsy. That’s why driving after taking one can be dangerous. That’s why older adults are at higher risk of falls. And that’s why even a short course can lead to dependence.
When They’re Used - And When They’re Not
Doctors don’t hand out benzodiazepines like candy. They’re prescribed for very specific, short-term situations:
- Acute panic attacks - especially when SSRIs haven’t kicked in yet (which can take weeks)
- Alcohol withdrawal - to prevent seizures and delirium
- Seizure emergencies - like status epilepticus, where every second counts
- Procedural sedation - before surgery or colonoscopies
- Severe insomnia - but only for a few nights, not months
They’re not meant for daily, long-term use. Yet, that’s exactly what happens. In 2021, over 76 million benzodiazepine prescriptions were filled in the U.S. alone. About 12.6% of adults got at least one. Women are prescribed them more often than men. And while they work fast, their usefulness fades fast.
After just 2-4 weeks of daily use, your brain starts adapting. The same dose stops working as well. That’s tolerance. And when tolerance builds, people often take more - not realizing they’re walking into dependence.
The Dependence Trap
Dependence doesn’t mean you’re addicted. It means your body has changed. You need the drug to feel normal. Stop it suddenly, and your nervous system goes into overdrive. That’s withdrawal.
Up to 50% of people who take benzodiazepines daily for more than four weeks develop physical dependence. That’s not rare. That’s expected. Withdrawal symptoms can include:
- Rebound anxiety - worse than before you started
- Insomnia that won’t quit
- Tremors, sweating, heart palpitations
- Seizures - in severe cases
- Memory gaps, hallucinations, feelings of unreality
People on Reddit’s r/Anxiety forum say they felt “like their brain was on fire” after stopping. Others describe months of brain zaps, dizziness, and emotional numbness. One study found 23% of users had memory gaps during normal activities - forgetting conversations, driving routes, even meals.
The Ashton Manual, the gold standard for tapering off benzodiazepines, says most people need 3-6 months to safely stop after long-term use. Some need over a year. And that’s with medical supervision. Doing it alone? That’s how people end up in emergency rooms.
Who’s at Highest Risk?
Not everyone who takes benzodiazepines ends up dependent. But some groups are far more vulnerable:
- People over 65 - they’re 50% more likely to fall and 32% more likely to develop dementia with long-term use
- Those with a history of substance use - alcohol, opioids, or stimulants
- People using them for more than 4 weeks without a clear exit plan
- Those taking multiple sedatives - like mixing benzos with sleep aids or alcohol
The American Geriatrics Society says these drugs should be avoided entirely in older adults. The UK’s NICE guidelines now say they shouldn’t even be started for anxiety. And the FDA added a boxed warning in 2020 - the strongest kind - about abuse, addiction, and life-threatening withdrawal.
What Works Better in the Long Run
If you’re dealing with chronic anxiety or insomnia, benzodiazepines aren’t the answer. They’re a bandage on a broken bone.
For anxiety, SSRIs and SNRIs - like sertraline or venlafaxine - take 4-6 weeks to work. But once they do, they last. And they don’t cause dependence. For insomnia, CBT-I (Cognitive Behavioral Therapy for Insomnia) is more effective than any sleep pill, long-term. It teaches your brain how to sleep again - without drugs.
And here’s the best part: combining low-dose benzodiazepines with CBT reduces long-term dependence risk by 58%, according to a 2023 JAMA study. That’s not a coincidence. It’s a strategy.

What to Do If You’re Taking Them
If you’re on benzodiazepines right now, here’s what matters:
- Don’t stop cold turkey. That’s dangerous. Seizures can happen.
- Ask your doctor about a taper plan. Reduce by 5-10% every 1-2 weeks. Slower is safer.
- Use a long-acting benzo like diazepam for tapering - it’s easier on your system than short-acting ones like alprazolam.
- Track your symptoms. Keep a journal. Note mood, sleep, energy. It helps your doctor adjust your plan.
- Explore non-drug options. Therapy, exercise, mindfulness - these aren’t alternatives. They’re foundations.
Many people who’ve successfully tapered say the hardest part wasn’t the physical symptoms. It was the fear. Fear that the anxiety would come back. Fear they’d lose control. But with support, most find they don’t need the drug anymore. Their brain readjusts. Their natural GABA system heals.
The Bigger Picture
Benzodiazepines aren’t going away. They’re still vital in emergencies. In ICUs. In ERs. For people having seizures. For those going through alcohol detox.
But their role is shrinking. Prescriptions are projected to drop 15-20% over the next decade. More doctors are learning to say no. More systems, like Kaiser Permanente, are using electronic alerts to block prescriptions longer than 90 days.
The message is clear: these drugs save lives - but only when used correctly. Short-term. With supervision. With a plan to stop.
They’re not a solution for lifelong anxiety. They’re a bridge - and bridges are meant to be crossed, not lived on.
Can you get addicted to benzodiazepines if you take them as prescribed?
Yes. Physical dependence can develop even when taken exactly as directed. After just 2-4 weeks of daily use, your brain adapts. That’s not addiction - it’s physiology. Addiction involves compulsive use despite harm. Dependence means your body needs the drug to avoid withdrawal. Many people who become dependent never misuse their pills. That’s why doctors now limit prescriptions to short durations.
What’s the difference between short-acting and long-acting benzodiazepines?
Short-acting ones - like triazolam or alprazolam - work fast and wear off quickly. They’re good for panic attacks or short-term insomnia but cause more withdrawal symptoms when stopped. Long-acting ones - like diazepam or clonazepam - stay in your system longer. They’re better for tapering off and managing chronic conditions like epilepsy or alcohol withdrawal. But they can cause next-day drowsiness and are riskier for older adults.
Are there safer alternatives to benzodiazepines for anxiety?
Yes. SSRIs (like sertraline) and SNRIs (like venlafaxine) are first-line for long-term anxiety. They take weeks to work but have no addiction risk. For insomnia, CBT-I is more effective than any sleep pill over time. For acute panic, breathing techniques and grounding exercises can help. And combining therapy with very low-dose benzos reduces dependence risk by over half, according to JAMA Internal Medicine.
Why do benzodiazepines cause memory problems?
They interfere with the brain’s ability to form new memories - a side effect called anterograde amnesia. This happens at therapeutic doses. People forget conversations, where they put things, or even parts of their day. It’s not just “getting forgetful.” It’s a direct effect on the hippocampus, the part of the brain responsible for memory formation. This is why they’re used in medical procedures - you won’t remember the surgery. But it’s risky if you’re driving or managing daily tasks.
Is it safe to take benzodiazepines with alcohol or opioids?
No. Never. Combining benzodiazepines with alcohol, opioids, or other sedatives can slow your breathing to dangerous levels - even stopping it completely. This is how many overdoses happen. The FDA and CDC both warn that this combination is one of the leading causes of drug-related deaths. Even a single drink with a benzo can be risky. If you’re prescribed one, avoid alcohol entirely.
How long does benzo withdrawal last?
It varies. Acute withdrawal - with symptoms like anxiety, tremors, and insomnia - usually peaks in the first 2 weeks and fades over 4-8 weeks. But some people experience protracted withdrawal - lingering symptoms like brain fog, dizziness, or emotional sensitivity - for months or even over a year. This is why tapering slowly under medical care is essential. The Ashton Manual recommends reducing doses by 5-10% every 1-2 weeks. Rushing it makes withdrawal worse.
If you’re considering stopping benzodiazepines, talk to your doctor. Don’t wait until you’re in crisis. There’s a path out - and you don’t have to walk it alone.






13 Comments
I took lorazepam for three months after my mom died. Thought it was helping. Turns out I was just numbing the grief. When I tried to quit, I had panic attacks so bad I thought I was dying. Took me eight months to taper. No one warned me. Don’t let them gaslight you into thinking it’s ‘just anxiety.’ It’s your brain screaming for balance.
While the empirical data presented regarding GABAergic modulation is statistically significant, one must interrogate the underlying epistemological framework of pharmaceutical interventionism. The pharmacological suppression of affective states, while temporally efficacious, fundamentally undermines the phenomenological imperative toward existential integration. In other words: you’re not healing-you’re medicating away the signal.
Y’all need to hear this: benzos are like a fire extinguisher for your brain. 🔥🪣 You don’t live in the firehouse. I used to take alprazolam like candy until I started forgetting my own birthday. Then I found CBT-I and therapy. Not magic. Not easy. But real. My brain’s been quiet for 2 years now. No pills. Just me, my journal, and a damn good walk every morning. 🌿 You got this.
ok so i just got prescribed clonazepam for panic and i thought it was a godsend but now im scared bc i read this and now i think im gonna turn into a zombie who forgets where she put her keys and also her cat? 😵💫 i dont wanna be that person. any advice? i just wanna chill without being a mess.
Just wanted to say thank you for this. I’ve been on benzos for 6 years. Started with one pill a week, now I’m on 3 a day. I didn’t realize how much I’d lost until I started tapering. My memory came back slowly. My emotions too. I cried for three weeks straight when I stopped. But I’m not scared anymore. I’m just… me. And that’s enough.
It’s not merely about dependence-it’s about the cultural capitulation to chemical convenience. We’ve outsourced our emotional labor to pharmaceutical corporations who profit from our inability to sit with discomfort. The fact that 76 million prescriptions were filled in a single year isn’t a medical statistic-it’s a moral failure of the healthcare system, the insurance industry, and the collective psyche of a society that equates relief with resolution.
Oh please. The FDA ‘boxed warning’? That’s just regulatory theater. You know what’s really dangerous? SSRIs causing suicidal ideation in teens. But no one’s banning those. Why? Because Big Pharma owns Congress. This whole anti-benzo crusade is just fearmongering to push you toward their new $800/month ‘magic’ antidepressants. Wake up.
Wow. Such a thoughtful, nuanced, and completely unhelpful essay. I’m sure the 80-year-old woman who’s been on diazepam since 1998 because her doctor said ‘it’s fine’ really appreciates your 2000-word lecture on GABA receptors. Maybe next time, try writing for actual humans, not academic journal reviewers.
I’ve been sober from benzos for 18 months now. The first six were hell. Tremors. Nightmares. Feeling like my skin was crawling off. But I did it with therapy, a supportive partner, and a damn good therapist who didn’t judge me. I’m not saying it’s easy. I’m saying it’s possible. And if you’re reading this right now? You’re already stronger than you think.
Hey. I’m here. I’ve been where you are. If you’re scared to quit, that’s normal. But you don’t have to do it alone. Find a support group. Talk to your doctor. Write down how you feel every day. Small steps. One day at a time. You’re not broken. You’re just healing. And that’s beautiful. 💛
People who take benzos for anxiety are just lazy. Real strength is facing your fears without a chemical crutch. If you need a pill to get through the day, maybe you should’ve never been allowed to drive, vote, or breathe air without a permit. This isn’t medicine. It’s moral surrender.
I used to think the worst part of withdrawal was the physical symptoms-the tremors, the brain zaps, the insomnia. But the real horror? The loneliness. You feel like no one understands. Like your own mind betrayed you. I didn’t speak for months. Didn’t answer texts. Just sat. And waited. And slowly, the quiet returned-not because of a pill, but because I let myself be still. And in that stillness, I remembered who I was before the fear.