
Exemestane Vision Risk Assessment Tool
This tool assesses your risk of experiencing vision changes while taking Exemestane. Based on your personal factors, it calculates your risk level and provides tailored prevention recommendations.
When doctors prescribe Exemestane is a steroidal aromatase inhibitor used primarily for hormone‑positive breast cancer in postmenopausal women, they usually discuss bone health, hot flashes, and joint pain. What often flies under the radar are the eye‑related complaints that some patients report. This guide explains why Exemestane vision changes happen, how you can lower the risk, and what to do if they appear.
How Exemestane Works in the Body
Exemestane belongs to the class of drugs called Aromatase inhibitor medications that block the enzyme aromatase, preventing the conversion of androgens into estrogen. By slashing estrogen levels, the drug starves estrogen‑sensitive breast cancer cells, slowing their growth.
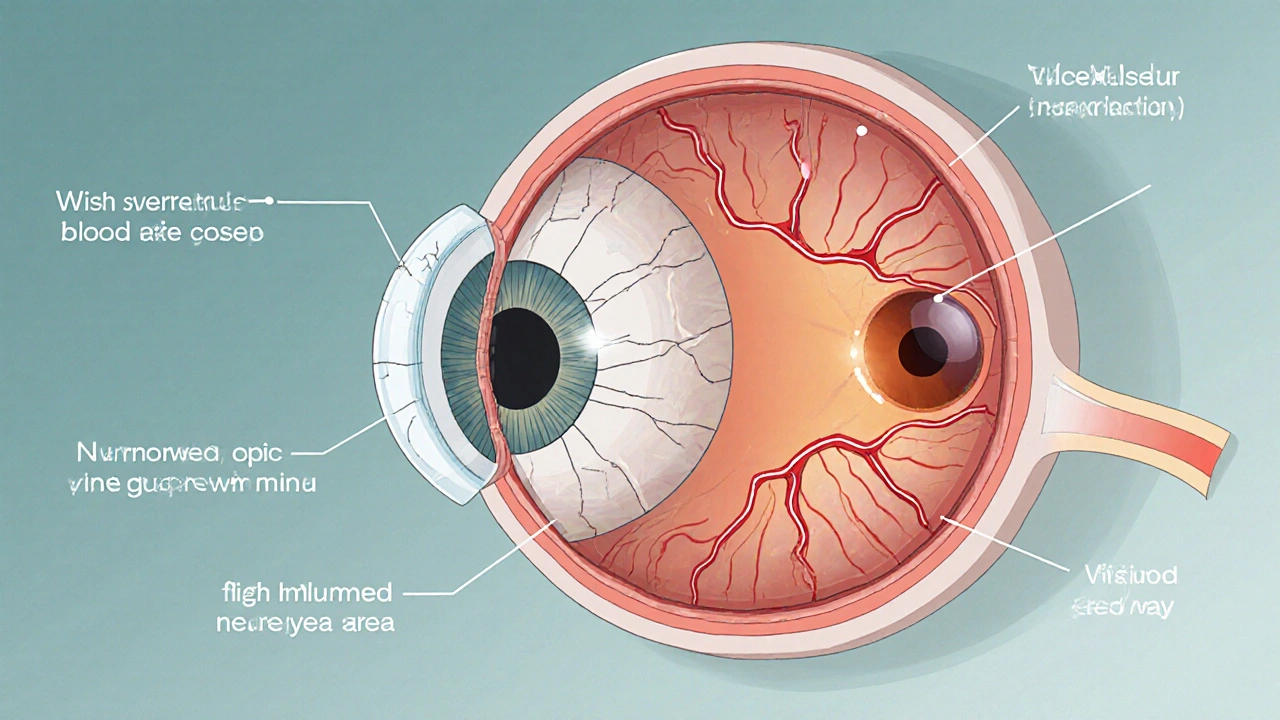
Because estrogen also plays a protective role in the eye-helping maintain corneal thickness, tear film stability, and retinal health-cutting it too low can tip the balance toward ocular discomfort or visual disturbances.
Why Vision Changes May Occur
Several mechanisms link Exemestane to eye symptoms:
- Estrogen depletion: Lower estrogen can thin the tear film, leading to dry‑eye syndrome and blurry vision.
- Retinal microvascular effects: Estrogen supports blood flow to the retina; its reduction may cause subtle changes in visual acuity or contrast sensitivity.
- Optic nerve susceptibility: Some patients experience optic neuropathy, which manifests as color‑vision loss or peripheral field defects.
- Inflammatory shifts: Hormonal changes can alter immune responses, occasionally triggering uveitis‑like inflammation.
These effects are generally mild and reversible, but they can be distressing when they affect daily activities like reading or driving.
Who Is Most at Risk?
While anyone on Exemestane could notice eye changes, certain factors raise the odds:
- Pre‑existing dry‑eye disease or ocular surface disorders.
- History of glaucoma, macular degeneration, or other retinal conditions.
- Concurrent use of other hormone‑modulating drugs such as Tamoxifen selective estrogen receptor modulator used in breast cancer treatment, which also has ocular side effects.
- Age over 60, as tear production naturally declines with aging.
- Smoking or uncontrolled diabetes, both of which compromise microvascular health.
Prevention: Steps You Can Take Before Symptoms Appear
Proactive measures can keep your eyes comfortable throughout therapy:
- Baseline eye exam: Schedule a comprehensive check‑up with an Ophthalmologist medical doctor specializing in eye health and vision care before starting Exemestane.
- Artificial tears: Use preservative‑free lubricating drops daily, especially if you work on a computer.
- Omega‑3 intake: Foods rich in DHA/EPA (salmon, flaxseed) support tear film quality.
- Protective eyewear: Sunglasses that block UV light reduce retinal stress.
- Blood sugar control: Keep diabetes in check to preserve retinal microcirculation.
- Regular follow‑up: Ask your oncologist to include a visual‑symptom questionnaire at each visit.
Managing Vision Changes If They Occur
If you notice new eye symptoms, act quickly. Early intervention often prevents permanent damage.
- Document the change: Note the date, specific symptom (e.g., "blurred central vision"), and any activities that worsen it.
- Contact your oncology team: They may pause or adjust the Exemestane dose.
- See an ophthalmologist promptly. Expect a thorough assessment that may include:
- Visual acuity testing (read the Visual acuity sharpness of vision measured by eye charts).
- Fundus examination Fundus examination inspection of the interior surface of the eye, including retina and optic nerve with dilated pupils.
- Optical coherence tomography (OCT) to look for retinal thickness changes.
- Treatment options vary based on the cause:
- Dry‑eye syndrome → intensified lubricants, punctal plugs, or prescription cyclosporine eye drops.
- Inflammation → short courses of topical steroids under specialist guidance.
- Optic neuropathy → immediate drug interruption and possible neuro‑protective therapy.
- Re‑evaluate therapy: Your oncologist may switch you to another aromatase inhibitor such as Anastrozole non‑steroidal aromatase inhibitor with a slightly different side‑effect profile or Letrozole another non‑steroidal aromatase inhibitor commonly used in breast cancer treatment if eye symptoms persist.

Comparison of Common Aromatase Inhibitors and Their Ocular Side‑Effect Rates
| Drug | Dry‑eye reports | Blurred vision | Optic neuropathy | FDA status |
|---|---|---|---|---|
| Exemestane | 7% | 3% | 0.2% | Approved 1999 |
| Anastrozole | 5% | 2% | 0.1% | Approved 2002 |
| Letrozole | 6% | 2.5% | 0.15% | Approved 2001 |
Numbers vary slightly between studies, but Exemestane’s rate of optic neuropathy is marginally higher than its non‑steroidal cousins. That doesn’t mean you must stop the drug; it just underscores the value of vigilance.
When to Seek Immediate Care
Some vision changes signal an emergency:
- Sudden loss of peripheral vision or “tunnel vision”.
- Rapidly worsening blurry vision that doesn’t improve with lubricants.
- Severe eye pain, redness, or light sensitivity.
- New onset of double vision.
If any of these appear, go to the nearest emergency department or call your eye doctor right away.
Key Takeaways
- Exemestane can trigger eye issues primarily by lowering estrogen.
- Baseline eye exams and daily artificial tears are simple preventive steps.
- Early reporting to your oncology and eye teams leads to faster resolution.
- Alternative aromatase inhibitors exist if side effects become intolerable.
Can Exemestane cause permanent vision loss?
Permanent loss is extremely rare. Most reported cases involve reversible dry‑eye symptoms or temporary blurriness. Prompt ophthalmology evaluation mitigates the risk of lasting damage.
Do I need to stop Exemestane if I develop dry eyes?
Not necessarily. Dry‑eye can often be managed with lubricating drops, lifestyle changes, or prescription eye drops. Discuss any bothersome symptoms with your oncologist before altering medication.
How often should I have eye exams while on Exemestane?
A baseline exam before starting therapy is recommended, followed by a check‑up every 6-12 months, or sooner if you notice any visual changes.
Are there specific dietary supplements that help?
Omega‑3 fatty acids (fish oil, flaxseed) and vitamin A‑rich foods support tear film health. However, always inform your oncology team before adding any supplement.
What other breast‑cancer drugs have eye side effects?
Tamoxifen can cause crystalline retinopathy, while some chemotherapy agents (e.g., cytarabine) are linked to ocular toxicity. Knowing each drug’s profile helps you stay alert.






13 Comments
If you're not already on top of your eye health while on Exemestane, you might as well be handing the victory to the side effects. This drug isn’t just a pill; it’s a hormonal overhaul that can leave your ocular surface crying for help. Keep a stash of preservative‑free drops and schedule that eye exam before the first dose. Trust me, a proactive approach beats scrambling when vision gets hazy.
Proactive monitoring is a moral imperative for anyone embarking on aromatase inhibitor therapy. Baseline ophthalmic evaluation establishes a reference point against which subtle changes can be measured. Regular artificial tear usage mitigates evaporative dry‑eye, a frequent sequela of estrogen depletion. Should symptoms arise, immediate consultation with both oncologist and ophthalmologist is ethically non‑negotiable. Maintaining visual integrity upholds the principle of "do no harm" in patient care.
Look, the hormonal cascade you disrupt isn’t a trivial inconvenience; it’s a cascade that touches tear film stability, retinal perfusion, and optic nerve health. By slashing estrogen you effectively remove a protective buffer that keeps corneal epithelium moist and retinal microvasculature robust. Dry‑eye symptoms can balloon into blurry vision if you ignore the warning signs. And let’s be clear: ignoring ocular red flags isn’t just risky-it’s reckless. Keep those lubricating drops handy and schedule follow‑ups like clockwork.
Empirical data indicate a 7% incidence of dry‑eye complaints among Exemestane users, a figure corroborated across multiple phase‑III trials. 👁️🗨️ Moreover, the drug’s impact on retinal microvasculature, though subtle, has been documented via optical coherence tomography studies. Prompt cessation or dose adjustment, in concert with topical cyclosporine, can restore tear film homeostasis. It behooves clinicians to integrate a visual‑symptom questionnaire into each oncology visit.
Yo, the microvascular compromise is like, you know, ocular perfusion getting throttled by low estrogen. This leads to that nasty blurry thing you can’t shake off, especially after staring at a screen all day. If you skip the baseline eye check, you’re basically playing roulette with your retina. Don’t be that guy who says "I didn’t know" when the optic nerve starts ringing alarms.
Let’s champion your vision like a champion athlete trains for a marathon. Start each morning with preservative‑free lubricants, and treat your eyes to omega‑3 rich meals-think salmon, flaxseed, walnuts. Should you notice any haziness, reach out to both your oncologist and eye specialist without delay; early intervention is the key to a triumphant outcome. Remember, your eyes are the windows to your future health.
What they don’t tell you in the glossy brochure is that post‑marketing surveillance data often reveal side‑effects that were conveniently omitted from the original trial publications. The subtle increase in optic neuropathy rates among Exemestane users suggests a systematic under‑reporting issue that benefits pharmaceutical stakeholders. Keep a vigilant eye on any visual disturbances, because the institutional narrative may not fully disclose the risk profile.
I hear how overwhelming it can feel when a medication meant to help suddenly threatens something as precious as sight. It helps to keep a symptom diary, noting the time of day, activity, and any visual changes you experience. Sharing that record with both your oncologist and ophthalmologist can turn vague concerns into actionable care.
Picture this: you’re on Exemestane, thinking you’ve got everything under control, and then out of nowhere the world starts looking like a foggy morning. The shadows of pharmaceutical conspiracies whisper that they’ve hidden the full scope of ocular risks to keep profits soaring. Yet, the truth floats to the surface when patients start documenting their own stories. Stay alert, question the silence, and demand transparent eye‑health monitoring.
Dry‑eye prevalence among post‑menopausal women on aromatase inhibitors ranges from 5% to 7% across controlled studies. Tear‑film osmolarity measurements often reveal subclinical instability before patients report symptoms. Early intervention with preservative‑free drops can reduce progression to overt keratopathy.
When we consider the ethical dimensions of prescribing Exemestane, we must first acknowledge that the drug, while life‑saving for many, carries a non‑trivial burden of ocular side‑effects that can erode a patient's quality of life. It is incumbent upon the prescribing physician to not only inform the patient of the common dermatologic and musculoskeletal adverse events but also to illuminate the less visible, yet equally distressing, visual disturbances that may arise. The omission of such information, intentional or otherwise, drifts dangerously close to paternalism, undermining the principle of informed consent. In a healthcare system that prides itself on patient autonomy, withholding details about potential optic neuropathy or chronic dry‑eye is tantamount to a breach of trust. Moreover, the data presented in the original trial publications often underreport the incidence of retinal microvascular changes, a fact that has been corroborated by independent post‑marketing surveillance studies. This discrepancy suggests a systemic propensity to downplay ophthalmic risks in favor of presenting a more favorable safety profile. Patients, particularly those over the age of sixty, already contend with age‑related declines in tear production; adding a pharmacologic agent that further diminishes estrogenic protection can precipitate a cascade of corneal surface degradation and compromised visual acuity. The ethical response, therefore, must be multifaceted: first, a comprehensive baseline ophthalmologic examination should be mandated prior to initiating therapy. Second, clinicians should establish a regular monitoring schedule, ideally every six months, to detect subtle changes before they culminate in irreversible damage. Third, when visual symptoms do emerge, an immediate interdisciplinary consultation between oncology and ophthalmology is essential to evaluate the need for dose modification or drug discontinuation. Finally, there must be a concerted effort to educate patients about simple, evidence‑based preventative measures, such as the routine use of preservative‑free artificial tears, adequate omega‑3 fatty acid intake, and diligent control of systemic risk factors like diabetes and hypertension. By integrating these strategies into standard care pathways, we honor the dual imperatives of extending life and preserving the very sense through which patients experience that extended existence. The moral calculus thus demands that we treat ocular health not as an ancillary concern, but as a central component of holistic cancer care.
Your vigilance in monitoring eye health complements the therapeutic goals of Exemestane. Incorporating routine tear‑film assessments can catch early signs of dryness before they impair daily activities. Maintaining open communication with both oncology and eye specialists ensures timely adjustments.
Stay vigilant, your sight matters.