Narrow therapeutic index drugs are not like most medications. For these drugs, the difference between the right dose and a dangerous one is razor-thin. A little too much can land you in the hospital. A little too little might mean your condition comes back with a vengeance. There’s no room for guesswork. If you’re taking one of these drugs, understanding how they work - and what you need to do - isn’t optional. It’s life-saving.
What Exactly Is a Narrow Therapeutic Index Drug?
A narrow therapeutic index (NTI) drug has a very small window between the dose that works and the dose that harms you. Think of it like walking a tightrope. One step too far to the left, and you don’t get the benefit. One step too far to the right, and you risk serious harm - even death.
The U.S. Food and Drug Administration (FDA) defines NTI drugs as those where small changes in blood levels can cause serious problems: life-threatening reactions, permanent disability, or treatment failure. For most drugs, your body can handle a little variation. Not with NTI drugs. A 10% to 20% increase in your blood concentration can push you from safe to toxic.
These drugs are measured by their therapeutic index - the ratio between the dose that causes toxicity and the dose that gives the desired effect. If that ratio is less than 2:1, it’s classified as NTI. For comparison, most drugs have a ratio of 10:1 or higher. That’s why NTI drugs need special care.
Common NTI Drugs You Might Be Taking
You might not realize you’re on an NTI drug - many are prescribed for chronic conditions. Here are the most common ones:
- Warfarin (Coumadin, Jantoven): Used to prevent blood clots. Your blood’s clotting time is measured by INR. The target range is 2.0-3.0. Above 3.5? Risk of dangerous bleeding. Below 2.0? Risk of stroke or clot.
- Lithium (Lithobid): Used for bipolar disorder. Therapeutic range: 0.6-1.2 mmol/L. Above 1.5? Tremors, confusion, seizures. Below 0.6? Mood episodes return.
- Levothyroxine (Synthroid): For hypothyroidism. Even small changes in dose can throw off your TSH levels. A switch in generic brands has caused TSH to jump from 1.8 to 8.4 in some patients - leading to fatigue, weight gain, and depression.
- Digoxin (Lanoxin): For heart failure and irregular heartbeat. Therapeutic range: 0.5-0.9 ng/mL. Above 2.0? Life-threatening heart rhythms.
- Tacrolimus (Prograf): Used after organ transplants. Too low? Organ rejection. Too high? Kidney damage. Levels must be checked often, especially early after transplant.
- Phenytoin (Dilantin) and Carbamazepine (Tegretol): For seizures. Blood levels must stay in a tight range to prevent seizures or toxicity like dizziness, nausea, or even coma.
- Methotrexate (Trexall): Used for autoimmune diseases and some cancers. Small changes can cause severe bone marrow suppression or liver damage.
There’s no official FDA list of all NTI drugs. Instead, experts use clinical guidelines, drug monitoring requirements, and documented overdose outcomes to identify them. If your doctor orders regular blood tests for your medication, it’s likely an NTI drug.
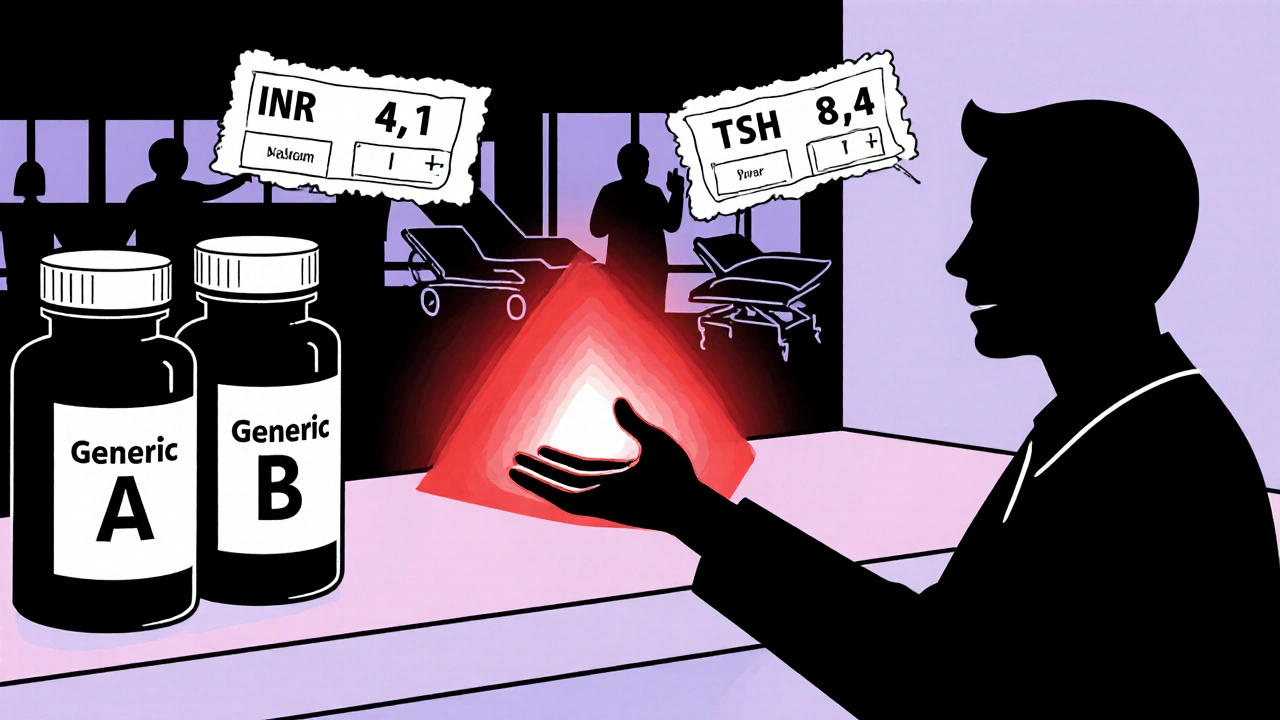
Why Generic Switches Can Be Dangerous
Many patients assume generics are interchangeable with brand-name drugs. With most medications, that’s true. With NTI drugs, it’s not always safe.
Generic versions must prove they’re “bioequivalent” - meaning they deliver the same amount of drug into your bloodstream as the brand. For most drugs, that means the generic’s absorption can be 80% to 125% of the brand. That’s a 45% range.
For NTI drugs, the FDA and European Medicines Agency (EMA) require a much tighter range: 90% to 111%. That cuts the variation from 45% to under 23%. But even that small difference can matter.
Real-world examples prove it:
- A warfarin patient switched from brand Coumadin to a generic. Within a week, her INR jumped from 2.5 to 4.1 - a level that caused dangerous bleeding. She needed emergency vitamin K.
- A patient on levothyroxine switched between two generic brands. Her TSH level went from 1.8 to 8.4 in six weeks - enough to trigger severe fatigue and weight gain.
Some states, like North Carolina, now require pharmacists to get your doctor’s approval before switching your NTI drug to a generic. Why? Because the risk isn’t theoretical. A 2021 study found hospitalizations for NTI drug complications were 2.3 times higher when patients switched between generic manufacturers.
What You Must Do to Stay Safe
Managing an NTI drug isn’t just about taking your pill. It’s about active, consistent participation in your care.
1. Stick to the Same Brand or Generic
If your doctor prescribes a specific brand or generic, ask your pharmacist to fill it the same way every time. Don’t let them switch it unless you and your doctor agree. If you’re unsure, ask: “Is this the same version I’ve been taking?”
2. Never Skip Blood Tests
Regular monitoring isn’t optional. It’s your safety net.
- Warfarin: INR checked every 1-4 weeks, especially when starting or changing doses.
- Lithium: Blood levels checked every 3-6 months - more often when adjusting dose or if you’re sick.
- Tacrolimus: Twice weekly at first after transplant, then monthly or as directed.
- Levothyroxine: TSH tested every 6-8 weeks after a dose change, then every 6-12 months if stable.
Missing a test means flying blind. You might feel fine - until you’re not.
3. Know the Signs of Too Much or Too Little
Learn the early warning signs for your drug:
- Warfarin - Too high: Easy bruising, nosebleeds, blood in urine or stool, severe headaches.
- Warfarin - Too low: New swelling or pain in legs, chest pain, sudden shortness of breath.
- Lithium - Too high: Hand tremors, slurred speech, confusion, vomiting, muscle weakness.
- Levothyroxine - Too high: Rapid heartbeat, weight loss, nervousness, insomnia.
- Levothyroxine - Too low: Fatigue, weight gain, cold intolerance, depression.
If you notice any of these, call your doctor. Don’t wait.
4. Track Your Medication and Symptoms
Keep a simple log: date, time, dose taken, symptoms, lab results. Apps approved by the FDA can help with this. Patients who track their meds and symptoms have 32% fewer adverse events.
5. Watch What You Eat and Drink
Some foods and supplements interfere with NTI drugs:
- Warfarin: Avoid large amounts of leafy greens (kale, spinach) - they’re high in vitamin K and can lower your INR.
- Lithium: Don’t drastically change your salt intake. Low salt can raise lithium levels.
- Levothyroxine: Take it on an empty stomach. Wait at least 30-60 minutes before eating or taking calcium, iron, or antacids - they block absorption.
Always tell your doctor about new supplements, even “natural” ones. They can change how your drug works.
What’s Changing in NTI Drug Management?
The system is improving - but slowly.
The FDA launched its Safe Use Initiative in 2022, requiring barcode scanning for 12 high-risk NTI drugs in hospitals to prevent dosing errors. In 2023, they released new guidance on bioequivalence testing for 15 specific NTI drugs, including levothyroxine and digoxin.
Researchers are also looking at genetics. A study at UCSF found that two genes - CYP2C9 and VKORC1 - explain 40-60% of why some people need much higher or lower doses of warfarin. By 2026, genetic testing before starting certain NTI drugs may become standard, potentially cutting adverse events by 35%.
Drug monitoring is a growing market. It was worth $2.8 billion in 2022 and is projected to hit $4.7 billion by 2027. More labs, more tools, more awareness - but the burden still falls on you.
How Long Does It Take to Get Used to an NTI Drug?
Most patients need 3 to 6 months to fully understand how their drug works and how to manage it. It’s not just about remembering to take it. It’s about learning to listen to your body, recognizing patterns, and knowing when to speak up.
One patient on lithium shared: “I had three hospitalizations in two years before I started regular blood tests. Now, after 8 years of consistent monitoring, I haven’t been hospitalized once.”
That’s the difference between passive care and active management.
Final Thought: You’re Not Alone
NTI drugs are scary. But they’re manageable. Thousands of people take them safely every day. The key isn’t perfection - it’s consistency. Stick to the same version of your drug. Show up for your blood tests. Track your symptoms. Ask questions. Don’t assume anything.
If your doctor says your drug is an NTI drug, take it seriously. This isn’t just another pill. It’s a medication that demands your attention. And with the right habits, you can live well - safely - on it.
Are all generic drugs unsafe for NTI medications?
No, not all generics are unsafe. But they must meet stricter bioequivalence standards (90%-111%) than regular drugs. Even then, small differences in absorption can matter. The safest approach is to stick with the same brand or generic version your doctor approves - and never switch without consulting them.
Can I stop taking my NTI drug if I feel fine?
Never stop or change your dose without talking to your doctor. Feeling fine doesn’t mean your drug level is right. For drugs like lithium or levothyroxine, you might feel normal even when your levels are too high or too low. Blood tests are the only way to know.
Why do I need so many blood tests?
Because your body’s response to NTI drugs is unpredictable. Factors like diet, other medications, illness, or even stress can change how your body absorbs or breaks down the drug. Regular blood tests catch these changes before they cause harm.
What should I do if I miss a dose?
Don’t double up. Call your doctor or pharmacist right away. For drugs like warfarin or lithium, missing a dose can be as risky as taking too much. Your provider will tell you whether to skip it, take it late, or adjust your next dose.
Can I switch to a different generic if my insurance won’t cover the brand?
If your insurance denies coverage, talk to your doctor first. They can request a prior authorization or suggest an alternative generic that’s known to work for you. Never switch generics on your own. Even if two generics are labeled the same, they can have different inactive ingredients that affect absorption.
Are there new technologies to help manage NTI drugs?
Yes. The FDA has cleared mobile apps that help track doses, symptoms, and lab results. Some hospitals use barcode scanning to prevent dosing errors. In the future, genetic testing may guide your starting dose for drugs like warfarin and clopidogrel, making treatment more precise and safer.






14 Comments