
Every year, over 60,000 children under age 6 are treated in emergency rooms after accidentally swallowing medications stored improperly at home. That’s not a rare accident-it’s a preventable crisis. And it’s not just kids. Seniors confuse similar-looking pills. Teens pull pills from unlocked cabinets. Adults take expired drugs because they don’t know they’re no longer safe. The fix isn’t complicated: a simple, consistent medication storage checklist can cut these risks by nearly 90%.
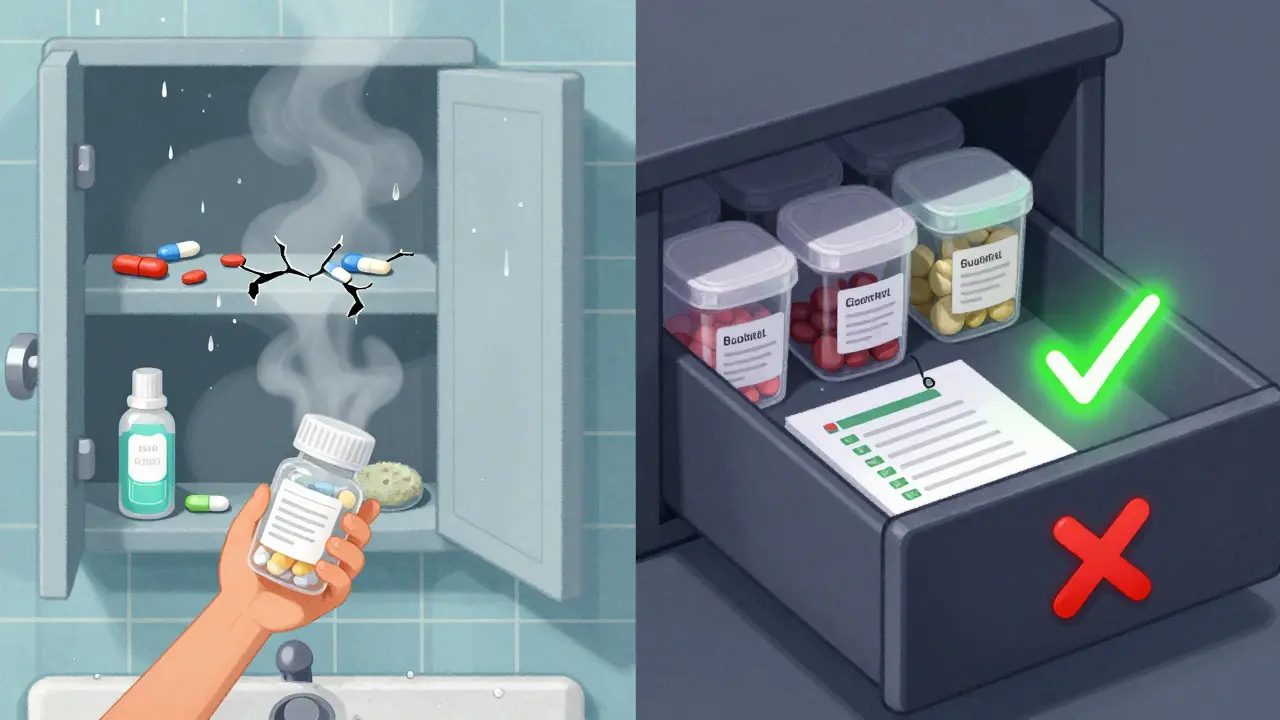
Start with the Right Location
Your bathroom cabinet is the worst place to store medicine. The heat from showers swings temperatures by 10-15 degrees. Humidity hits 80-90%. That’s enough to break down pills, creams, and inhalers in weeks. The FDA says light and moisture can reduce potency by up to 40% in just 30 days.Instead, pick a cool, dry, dark spot. A linen closet, a bedroom drawer, or a powder room with stable temperatures works best. Keep it between 68-77°F (20-25°C) and humidity under 60%. Use a small digital thermometer and hygrometer to check daily. If you’re storing insulin or other refrigerated meds, keep them at 36-46°F. Don’t put them in the fridge door-temperatures there bounce too much. Use the back shelf.
Lock It Down
Standard medicine cabinets? They’re useless against curious kids. Consumer Product Safety Commission tests show they block only 12% of access attempts. A 2023 Pediatrics study found households using locked medicine lockboxes saw 92% fewer accidental ingestions in children under 5.Don’t rely on high shelves alone. Kids climb. They open drawers. They watch you. Store medications behind three closed doors if possible-like inside a locked cabinet in a closet, then inside a closed closet door, then behind a bedroom door. For high-risk meds like opioids, insulin, or blood thinners, use a lockbox with a combination lock. They’re 34% more reliable than key locks because no one forgets the code.
Separate, Label, and Organize
Mixing medications is dangerous. One person’s painkiller shouldn’t be next to another’s blood pressure pill. The Institute for Safe Medication Practices found that separating meds by household member reduced wrong-medication errors by 63%.Use clear bins or small boxes. Label each with the person’s name. Group by type: oral pills, topical creams, inhalers, injectables. Keep all medications in their original bottles with pharmacy labels. That’s not just for looks-it’s the law in places like North Carolina under Kaitlyn’s Law. Labels tell you the name, dose, and expiration date. If a bottle’s missing, write the info clearly on the container with a permanent marker.
High-alert meds like warfarin, insulin, or opioids need extra attention. Add a red sticker that says “HIGH ALERT.” Store them in a separate locked container, even if the rest are in one box. One mistake with these can be fatal.
Check Expirations Every Six Months
About 70% of homes keep at least one expired medication. The FDA says most pills are still safe one year past expiration if stored right. But after two years, potency drops to 65%. At three years, it’s down to 42%. That’s not just ineffective-it’s risky. A weakened antibiotic might not kill an infection. An expired EpiPen might not save a life.Set a calendar reminder for April 1 and October 1-right after daylight saving time changes. That’s when 47% of people remember to do household tasks, according to Johns Hopkins. Pull out every bottle. Check the expiration date. Look for changes: pills that are cracked, discolored, or smell odd. Creams that separate or smell sour. Inhalers that feel lighter than usual. If it looks wrong, toss it.
For multi-dose vials (like insulin or eye drops), write the date you opened them. Most lose potency after 28-56 days, even if the bottle says “use by 2027.”
Dispose of Expired or Unwanted Meds the Right Way
Never flush pills down the toilet. Never throw them in the trash without mixing them first. The EPA says 60-80% of pharmaceuticals in U.S. waterways come from flushing or dumping. That’s not just pollution-it’s a public health threat.Use a drug take-back program. The DEA runs National Prescription Drug Take Back Day twice a year-in April and October. Over a million pounds of meds were collected in 2022 alone. Find a local drop-off site through your pharmacy or police station. Many pharmacies now have permanent drop boxes.
If there’s no take-back option, mix the pills with something gross: coffee grounds, cat litter, or dirt. Use a 1:3 ratio-three parts dirt to one part pills. Put it in a sealed container. Toss it in the trash. This reduces accidental ingestion by 76%, according to the FDA. Never crush pills before mixing-some can release dangerous fumes.

Special Cases: Insulin, Inhalers, and More
Insulin: Keep unopened vials in the fridge. Once opened, most can stay at room temperature for 14-56 days, depending on the type. Write the opening date on the vial. Store it away from direct sunlight-even on a windowsill can ruin it.Inhalers: Keep them in a plastic case or box to prevent accidental pressing. Humidity can clog the nozzle. Don’t store them in the bathroom. Cold weather can affect spray pressure-keep them indoors.
Topical products: Creams, lotions, and even bug spray count as medication under North Carolina’s Kaitlyn’s Law. Store them with your other meds, not in the shower. A child might mistake sunscreen for medicine-or vice versa.
Make It a Habit
A checklist only works if you use it. Here’s your simple monthly and biannual routine:- Monthly: Do a quick visual check. Look for new pills, missing bottles, or changes in color/texture.
- Weekly: Check fridge temperature if you store meds there. Log it in a notebook or phone app.
- Every 6 months: Full inventory. Remove expired meds. Reorganize. Update labels.
Keep your checklist printed and taped to the inside of the storage cabinet. Or save it as a note on your phone. Use checkboxes. Tick them off. Make it part of your routine, like changing smoke detector batteries.
Households that use a formal storage system report 89% fewer medication errors, according to Consumer Reports. That’s not just peace of mind-it’s safety. For kids. For seniors. For everyone who depends on these pills to stay healthy.
Can I store all my medications in one place?
Yes, but only if they’re properly separated. Store each person’s meds in their own labeled bin or drawer. Keep high-risk drugs like opioids and insulin in a separate locked container. Never mix prescriptions with over-the-counter pills or supplements unless they belong to the same person and are clearly labeled.
What if I don’t have a lockbox?
Use a small lockable tool box, a locked filing cabinet, or even a locked suitcase. The goal is to make access difficult for children and unauthorized users. A simple combination lock from a hardware store works. Avoid cheap plastic boxes with snap lids-they’re easy for kids to open.
Are expired medications dangerous to take?
Most aren’t toxic, but they may not work. An expired antibiotic could fail to treat an infection. An expired EpiPen might not stop anaphylaxis. For life-saving drugs, always replace expired ones. For pain relievers or antacids, potency drops over time-but they’re unlikely to harm you. Still, if it looks or smells off, throw it out.
How do I know if a medication has gone bad?
Look for these signs: pills that are cracked, discolored, or sticky; liquids that are cloudy or have particles; creams that separate or smell sour; inhalers that feel lighter than usual or don’t spray properly. If you’re unsure, don’t guess-discard it. The FDA says 53% of people can’t tell when meds are degraded without a checklist.
Should I keep old prescriptions just in case?
No. Keeping old prescriptions increases the risk of accidental use, confusion, or misuse. If you think you might need a drug again, talk to your doctor. Don’t rely on old bottles. Dosages change. Conditions change. Your body changes. Always get a new prescription instead of using leftovers.






10 Comments
so i just put all my meds in a shoebox under my bed and called it a day. my kid thinks it’s a treasure chest. she’s 3. she’s gonna be a pharmacist or a criminal. either way, we’re covered.
Let me just say, as someone who has spent 17 years meticulously organizing her pharmaceuticals by chemical compound, expiration date, and potential interaction risk-while also cross-referencing each with the FDA’s 2019 stability guidelines and the WHO’s 2021 storage advisory-this checklist is, frankly, underwhelming. I mean, sure, ‘cool, dry, dark’ is cute, but have you considered the vapor pressure of active pharmaceutical ingredients under fluctuating relative humidity? No? Then you’re not really solving the problem, you’re just... decorating it.
In India, we store medicines in a steel almirah, locked with a simple key. No fancy thermometers. No lockboxes. Just common sense and respect for the medicine. Children are taught from young age: this is not candy. It is not a toy. It is not for playing. We do not need a checklist to teach responsibility. We teach it through culture.
Oh wow, a checklist. How groundbreaking. I bet the FDA paid you to write this. Next you’ll be telling me to breathe in and out. I mean, really-‘use a digital hygrometer’? My grandma stored pills in a cigar box and lived to 98. Coincidence? I think not.
My mom used to keep all her meds in a Tupperware container labeled ‘Blessings.’ We didn’t know what was in it until she had a stroke and we found the insulin vials next to her anxiety pills. I wish I’d had this checklist back then. Just… please, if you’re reading this-label your stuff. Even if it’s just with a Sharpie. Even if it’s ugly. It matters.
Okay but have you seen the new lockboxes that sync with your phone? Like, you get a notification if someone opens it. And it’s only $22 on Amazon. I got one for my dad’s blood thinners. He thought I was overdoing it. Then he forgot to take his and tried to grab his wife’s blood pressure med. Yeah. We’re not taking chances anymore.
Expired meds are fine. Just crush them and flush. Problem solved.
Wow. This is so… American. In my family, we just take whatever’s left from last year’s cold. My uncle took his neighbor’s beta-blocker for his headache. He’s fine. Also, I keep my insulin in the glove compartment. It’s cold enough. And the car is locked. What’s the worst that could happen? My kid gets a free ride to the ER? We’ve been there. It’s not that bad.
Insulin should be stored in a controlled environment with ISO 15378 compliance. Your checklist is a toddler’s guide to pharmacology.
I just started using a pill organizer with time slots. It’s not perfect, but it’s helped me stop taking my husband’s blood pressure meds by accident. I think this checklist is helpful. Maybe not for everyone. But for me? It’s a lifeline.