
Ever wondered what really happens in your body after you take ibrutinib? It’s not something most people think about until they or someone they care about needs this cancer drug. Here’s the thing: knowing a bit about how your body handles ibrutinib can answer a lot of questions about why doses matter, why certain foods are off the table, or why you might need regular blood work.
After you pop that pill, ibrutinib gets going pretty fast. It’s absorbed in your gut and heads straight for your bloodstream. From there, it starts doing its job, but the story doesn’t stop at absorption. The way your body breaks it down and gets rid of it can affect how well it works and what side effects show up.
The fun (and sometimes tricky) part? Everyone processes this drug a bit differently. Have you ever noticed someone gets dizzy when you don’t? Or maybe one person has blood counts that dip, but you skate by without a hitch? That all ties back to how your body moves, changes, and clears ibrutinib. If you know those details, you’re one step ahead—ready to spot red flags or nudge your care in the right direction.
- How Ibrutinib Gets Absorbed
- What Your Liver Does with Ibrutinib
- Elimination: How Long Does It Stay in Your Body?
- Factors That Can Change Ibrutinib Levels
- Smart Tips for Taking Ibrutinib Safely
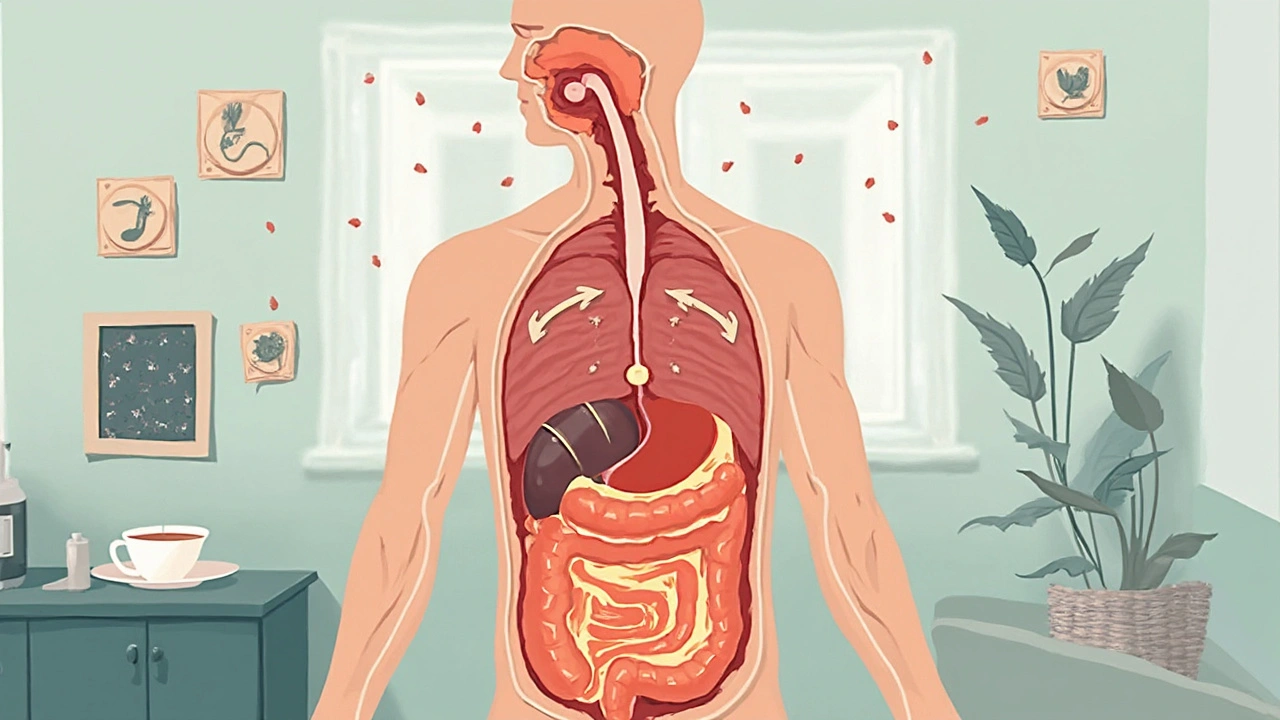
How Ibrutinib Gets Absorbed
After you swallow an ibrutinib capsule, it starts breaking down right in your gut. Most of the absorption happens in your small intestine. This is where the drug gets pulled into your bloodstream and heads out to where it’s needed. Here’s the kicker: on an empty stomach, your body absorbs ibrutinib pretty quickly—usually hitting its highest level in your blood about one hour after taking it.
Food can change the game, though. If you eat a big meal before taking ibrutinib, more of it gets into your system. This sounds good, but it actually means a bigger dose than expected, which could lead to stronger side effects. That’s why the pros say to take ibrutinib at the same time every day, either always with food or always without—just be consistent.
Hard to swallow pills? Here’s something to remember: Don’t crush, chew, or open ibrutinib capsules. Breaking them apart can mess up how much medicine you get, so you might end up with too little or too much in your body.
Check out these quick facts about ibrutinib's absorption:
- Best absorbed on an empty stomach, but always follow your doctor’s advice.
- Reaches peak blood levels in about 1-2 hours.
- Don’t mix with grapefruit or Seville orange juice—they can boost blood levels to risky territory.
If you’re sharing a bathroom with someone on ibrutinib, heads up: there’s no risk with touching their medications, but the person actually taking the drug should watch out for mixing up schedules, food, and other meds. Little things can make a big difference in how ibrutinib works.
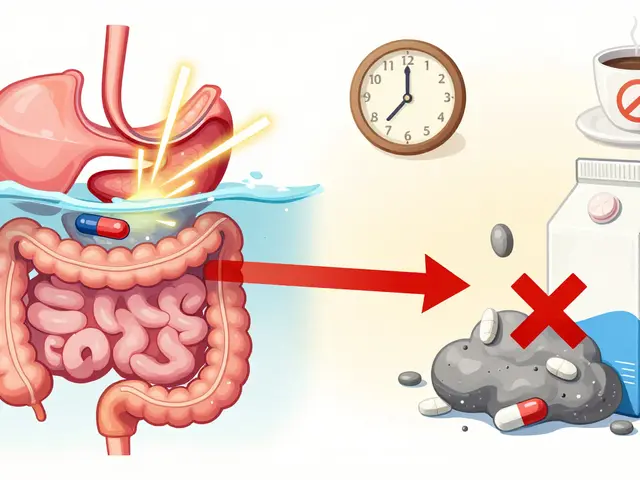
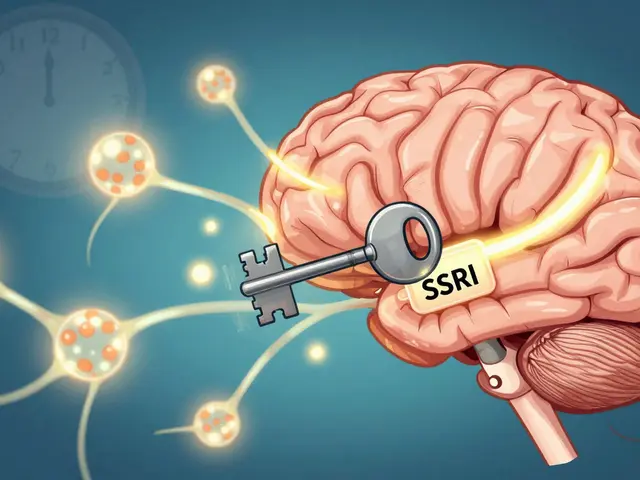
What Your Liver Does with Ibrutinib
Once ibrutinib gets into your bloodstream, your liver jumps in as the main boss. The liver uses a set of proteins—called enzymes—to break down the drug. The big player here is CYP3A4. If you’ve ever heard of people avoiding grapefruit with some meds, that’s usually because of this enzyme. CYP3A4 chews up ibrutinib into smaller pieces, which then move out of your system. If your liver isn't working well, or if you're taking something that messes with this enzyme, ibrutinib might stick around too long or disappear too fast.
It sounds technical, but this is a key reason why your doctor always wants a list of what you’re taking—including over-the-counter things, supplements, and even herbal teas. Some common meds, like certain antibiotics or anti-fungals, can block CYP3A4 and ramp up your ibrutinib levels, making side effects more likely. Others can rev up the enzyme, clearing the drug out before it can help you. So, no skipping the med list, even if you think something’s harmless!
“Ibrutinib is primarily metabolized in the liver via cytochrome P450 3A4, which means drug interactions and liver health play a huge role in how well it works and how safe it is.” — The Leukemia & Lymphoma Society
Let’s make it even clearer with a breakdown:
- Ibrutinib hits the liver after being absorbed.
- The enzyme CYP3A4 breaks ibrutinib down.
- Other drugs—and even some foods—can slow down or speed up CYP3A4.
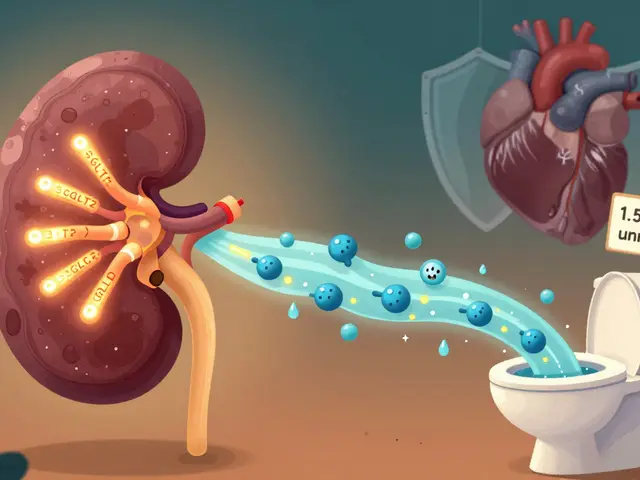
- The broken-down drug moves out through your pee and poop.
If you want to see how common some of these CYP3A4 blockers and boosters are, just look at this:
| CYP3A4 Blockers (Increase Ibrutinib) | CYP3A4 Boosters (Decrease Ibrutinib) |
|---|---|
| Grapefruit, Ketoconazole, Clarithromycin | St. John's Wort, Rifampin, Carbamazepine |
The bottom line? Your liver’s work with ibrutinib is a balancing act. Doctors often check your liver function with blood tests before and during treatment. If your liver is struggling, or if you’re on meds that mess with CYP3A4, your dose may need a tweak. Always check before adding any new pill, supplement, or even a "natural" remedy to your mix.
Elimination: How Long Does It Stay in Your Body?
If you’re taking ibrutinib, you might wonder: when does it actually leave your system? Turns out, this isn’t just a random detail—it can affect side effects, drug interactions, and how you plan your life around taking medicine.
Here’s how it works. After you swallow the dose, most of the drug gets processed quickly by your liver. The “half-life”—which means the time it takes for half the drug to leave your bloodstream—is about 4 to 6 hours for most people. So in less than a day, your blood level drops pretty low. But just because the drug fades from the bloodstream fast doesn’t mean its effects stop overnight. After a while, it’s more about the lasting impact on cancer cells than the amount swimming through your veins.
| Stage | Time |
|---|---|
| Peak Blood Level | 1-2 hours after taking |
| Half-Life | 4-6 hours |
| Mostly Gone | 24 hours |
Most of ibrutinib leaves your body in your poop (about 80%) and the rest in pee. What’s wild is you don’t actually pee out much that’s still “active”—your liver breaks it down into stuff your body can toss out easily.
“Ibrutinib is rapidly eliminated through hepatic metabolism, with a terminal half-life of less than 10 hours, primarily excreted in the feces.”
— U.S. FDA Prescribing Information
Keep in mind, other medicines you’re taking (especially ones that affect your liver), or if your liver isn’t working well, can slow down how fast you get rid of ibrutinib. That can mean levels stick around longer, raising your chances for side effects. Always check with your doctor before starting new meds—even over-the-counter stuff, like St. John’s wort or certain antibiotics, can mess with your body’s ability to clear the drug.
Factors That Can Change Ibrutinib Levels
Lots of things can shake up the amount of ibrutinib in your body. If you ever see one person have a different reaction or side effect than another, it probably comes down to what’s changing those drug levels. Sometimes, it’s simple stuff, like what you had for dinner, and other times it’s hidden in your medicine cabinet.
First up: food. Fatty foods can actually pump up the absorption of ibrutinib. That means a burger and fries might give you a bigger dose than you planned. But this isn’t always a good thing—too much absorption can lead to more side effects, like tummy trouble or headaches. Most doctors recommend taking it on an empty stomach for steady results, unless your pharmacist tells you otherwise.
Medications are a biggie, too. Some drugs mess with the enzymes in your liver, especially CYP3A4. If you take certain antibiotics (like clarithromycin) or antifungals (like ketoconazole), they can slow down how fast your liver chews through ibrutinib. That means more of the drug hangs around—raising your risk for side effects. On the flip side, things like rifampin speed up your liver, so the drug might not stick around long enough to help.
- High risk interactions: Antifungals, certain antibiotics, seizure meds, and even grapefruit juice (yep, really) can all affect your ibrutinib levels.
- Herbal supplements: St. John’s wort is one people forget about, but it can drop ibrutinib levels and make it less effective.
- Liver health: If your liver’s not working right from illness or injury, ibrutinib can build up in your system—it might last longer and hit harder.
- Age and genetics: Older folks sometimes process drugs more slowly, and your personal genes mean you might have a wild card in how your enzymes work.
Here’s a quick look at how some combos can affect ibrutinib pharmacokinetics:
| Factor | Effect on Ibrutinib | What Happens |
|---|---|---|
| Grapefruit juice | Raises levels | May cause extra side effects |
| Strong CYP3A4 inhibitors (antifungals) | Raises levels | More drug in your body, watch for toxicity |
| Strong CYP3A4 inducers (rifampin, St. John’s wort) | Lowers levels | Less effective treatment |
| High-fat meal | Raises absorption | Risk of more side effects |
| Liver disease | Raises levels | Prolongs drug exposure |
If you’re taking ibrutinib, give your care team a complete list of your meds and supplements. It’s way easier to keep levels safe when everyone knows what’s in your mix. And watch out for weird side effects—sometimes it means your drug level’s gone off track because something new got thrown in the mix.
Smart Tips for Taking Ibrutinib Safely
Taking ibrutinib isn’t just about swallowing a pill. Small habits can have a big impact on how well it works and how your body handles it. Let’s get into what helps you use this treatment safely and get the best shot at good results.
- Stick to a regular schedule. Try to take ibrutinib at the same time every day. Missing doses or bunching them up can mess with your blood levels and lower its effectiveness.
- Watch what you eat (and drink). Grapefruit and Seville oranges aren’t your friends while on ibrutinib. They mess with how your body breaks down the drug, which can make side effects worse.
- Heads up on other meds. Some antibiotics, antifungals, and even certain heart meds can interact with ibrutinib. Always check with your doctor or pharmacist before starting something new, even if it’s an over-the-counter pain reliever or herbal supplement like St. John’s wort.
- Don’t crush or chew the pills. Swallow them whole. Chewing or breaking them apart can mess with how your body absorbs the medication.
- Stay hydrated. Drink plenty of water to help your kidneys do their job and flush out anything your body doesn’t need.
- Keep up with blood tests. Blood counts and liver tests help spot trouble early. If the numbers take a turn, your care team can react fast.
If you forget a dose, don’t double up unless your doctor tells you to. A skipped pill every now and then won’t wreck your treatment, but tell your team if it keeps happening.
You’ll want to flag certain symptoms fast: unexplained bruising or bleeding, trouble breathing, fever, or severe diarrhea. These can be signs you need a dose change or more support. Don’t tough it out.
| Type | Examples | Effect |
|---|---|---|
| Foods | Grapefruit, Seville oranges | Boosts ibrutinib levels, can raise side effects |
| Medications | Antibiotics (clarithromycin), antifungals (ketoconazole), heart meds (diltiazem) | Can increase or decrease ibrutinib’s effect |
| Herbal supplements | St. John’s wort | Lowers ibrutinib levels, might make it less effective |
Keeping these tips in mind not only helps you avoid nasty surprises, but makes it more likely you’ll get the most from your ibrutinib treatment. Stay in the loop with your care team—open conversations lead to smoother sailing.



12 Comments
The pharmacokinetic profile of ibrutinib is a textbook case of how absorption variability can translate into clinical outcomes. When you take the pill on an empty stomach, the Cmax spikes within an hour, which can magnify adverse events if the patient isn’t monitored. Food, especially high‑fat meals, acts as a bio‑enhancer, pushing the AUC upward and potentially tipping the safety margin. Moreover, CYP3A4 inhibition by agents like ketoconazole can double systemic exposure, a fact that should never be overlooked. It’s essential for prescribers to map out every concomitant drug to avoid iatrogenic toxicity. In short, the kinetic dance of ibrutinib demands vigilant stewardship.
Hey folks, just wanted to add that the timing of the dose matters a lot. If you take it with a meal, you might see a higher level than expected – that can cause more side efecs. Also, watch out for grapefruit, it can pull the levels up way too high. In my clinic we always tell patients to keep a consistent routine – same time, same food situation. It helps the doc track how the drug is behaving. Hope that helps!
You must respect the dosing schedule or you risk sub‑therapeutic exposure, which is unacceptable. Take ibrutinib exactly as prescribed, at the same time each day, with or without food, but never change it on a whim. Failure to comply can lead to disease progression and increased toxicity. The pharmacology does not forgive laxity – it demands precision. In clinical practice, adherence is the cornerstone of success.
It's fascinating how a tiny capsule can set off a cascade of metabolic events. The liver's CYP3A4 acts like a gatekeeper, deciding how long the drug hangs around. Even subtle diet changes can tip the balance, reminding us that medicine is never isolated. Bottom line: consistency beats randomness every time.
In the grand theater of oncology, ibrutinib takes centre stage, yet many treat it as a mere cameo. The moral imperative is clear: we must honor the science behind its absorption, metabolism, and elimination. First, understand that an empty‑stomach intake yields a rapid peak, but consistency is the ethical backbone of therapy. Second, the cruel irony of grapefruit-nature's own saboteur-can elevate plasma concentrations to perilous heights, betraying the patient’s trust. Third, CYP3A4 inhibitors, those insidious pharmacokinetic villains, can double exposure, turning a life‑saving agent into a toxin. Fourth, inducers such as St. John's Wort stealthily diminish efficacy, a silent betrayal that no compassionate clinician can ignore. Fifth, the liver, our physiological alchemist, must be monitored; hepatic dysfunction is not a trivial footnote but a decisive factor in dosing. Sixth, the excretion route-80% fecal, 20% urinary-reminds us that renal considerations, though secondary, are nonetheless vital. Seventh, age and genetics sculpt a unique pharmacokinetic fingerprint for each individual, demanding personalized vigilance. Eighth, dietary fats, those seemingly benign companions, can amplify absorption, risking dose‑related toxicity. Ninth, the half‑life of 4‑6 hours underscores the necessity of strict adherence to avoid sub‑therapeutic gaps. Tenth, blood work is not a bureaucratic ritual but a moral covenant between patient and provider. Eleventh, the admonition against crushing pills is not pedantic; it preserves the drug's designed release profile. Twelfth, every missed dose is a breach of trust, a fissure in the therapeutic alliance. Thirteenth, proactive communication with the care team is a noble duty, not an optional courtesy. Fourteenth, the ultimate lesson is that ibrutinomab's pharmacokinetics are a symphony; we, as stewards, must conduct with unwavering fidelity. Finally, let us reject complacency, for in the realm of life‑threatening malignancies, there is no room for half‑hearted diligence.
🤔 Ever wonder why a high‑fat meal can turn a standard dose into a super‑dose? Your liver’s enzymes are like traffic cops, and certain foods or meds can either put up a roadblock or let everything speed by. 🍔🛑 If you’re on a keto plan, you might see higher levels-watch for extra nausea. 📈 Keep a log of what you eat and any new supplements; it’ll help your doc fine‑tune the regimen. 👍 Remember, staying hydrated supports renal clearance, even if most of the drug exits in the stool. 🌊 Lastly, never skip your blood counts-they’re the early warning system for trouble. Stay curious and stay safe! 🚀
Just a quick note: taking ibrutinib at the same time each day helps keep blood levels steady. 🍽️ If you eat grapefruit, it can boost the drug and cause more side effects, so it’s best avoided. 🛑 Also, don’t crush the tablets – the coating is important for how it works. 👍 Keep your appointments for blood tests, they keep an eye on how your liver is handling the medicine. 😊 Stay consistent and you’ll give yourself the best chance.
Take it same time everyday 😊
It’s unsettling how a simple pill can become a source of anxiety. When the side effects appear, the mind spirals, questioning every bite taken. A single missed dose feels like a betrayal of oneself. Yet, in the silence, we find a fragile resolve to keep going. The journey is both quiet and loud within.
Ibrutinib’s AUC is highly sensitive to CYP3A4 modulation. Grapefruit juice acts as a potent inhibitor, raising systemic exposure. Conversely, rifampin induces metabolism, reducing therapeutic levels. Dose adjustments must reflect these pharmacokinetic shifts. Monitoring plasma concentrations can mitigate adverse events. Precision dosing ensures optimal pharmacodynamic outcomes.
The half‑life of ibrutinib ranges between four and six hours. Food intake, especially fatty meals, can increase absorption. CYP3A4 inducers accelerate clearance, possibly compromising efficacy. Hepatic impairment prolongs exposure, demanding dose reductions. Routine liver function tests are therefore indispensable.
Consistency in dosing is key for maintaining therapeutic windows. Patients should avoid grapefruit and similar citrus to prevent unexpected spikes. Interaction with strong CYP3A4 inhibitors warrants close monitoring. Regular labs help catch any hepatic stress early, ensuring safe continuation of therapy.