
Medicines don’t just magically fix problems. They’re chemicals designed to interact with your body in very specific ways. Understanding how medicines work isn’t just for doctors - it’s the key to using them safely. When you know what a drug is doing inside you, you can spot warning signs, avoid dangerous mix-ups, and feel more in control of your health.
How Medicines Work: The Lock-and-Key System
Your body is full of tiny receptors - like locks - on the surface of cells. Medicines act as keys. Some keys turn the lock and activate a process (these are called agonists). Others block the lock so nothing else can fit (these are antagonists). This is the core idea behind a drug’s mechanism of action.
Take SSRIs like fluoxetine (Prozac). They don’t create more serotonin. Instead, they block the transporter that normally pulls serotonin back into nerve cells after it’s released. That leaves more serotonin floating around, helping mood regulation. It’s like putting a cork in a recycling tube - the signal stays active longer.
Aspirin works differently. It permanently disables an enzyme called COX-1, which makes chemicals that cause pain and swelling. That’s why one pill can reduce fever, ease a headache, or even lower heart attack risk. But it also means your stomach lining loses some protection, which is why long-term use can cause irritation.
Some drugs are designed to target very specific proteins. Trastuzumab (Herceptin), for example, only works on breast cancer cells that overproduce the HER2 protein. Doctors test tumors first. If HER2 isn’t present, the drug won’t help. This precision cuts down useless treatments and side effects.
What Happens After You Swallow a Pill?
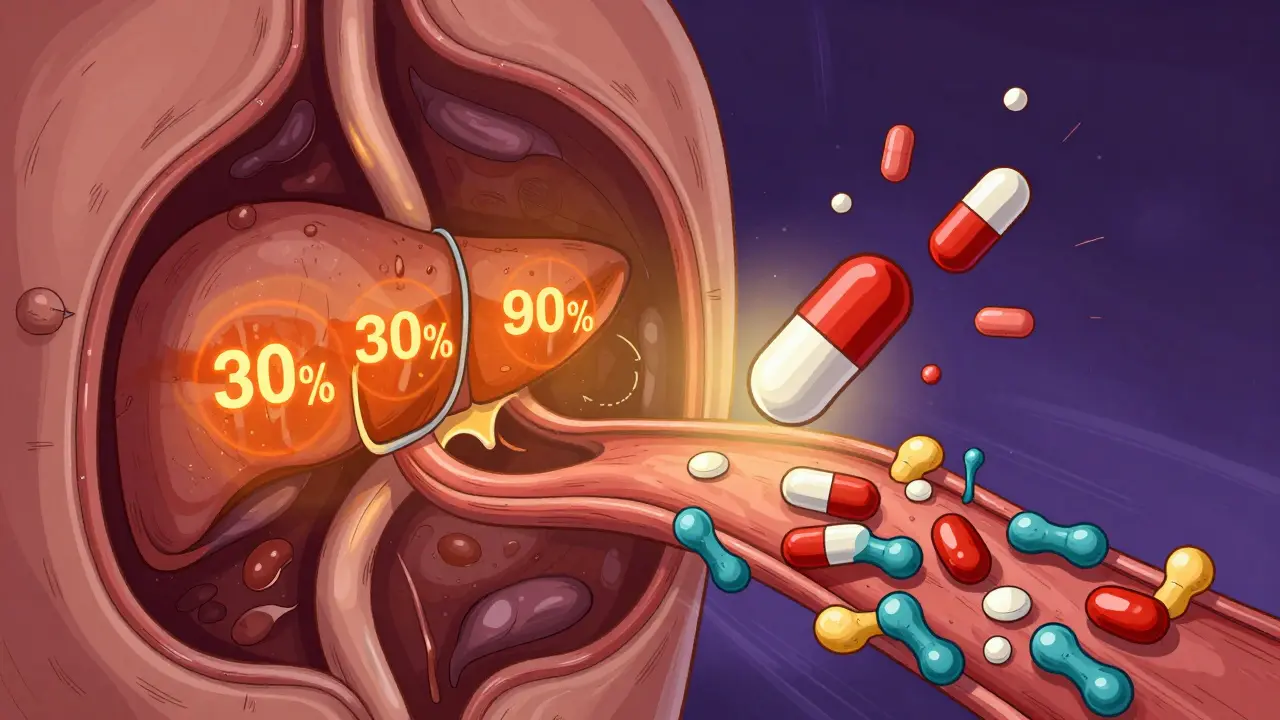
Not all medicines work the same way once they enter your body. Oral pills must survive your stomach acid, get absorbed through your gut, and then travel through your liver before reaching the rest of your bloodstream. This journey is called first-pass metabolism.
Some drugs, like morphine, lose about 30% of their strength during this trip. Others, like propranolol, can lose up to 90%. That’s why the same drug might have different doses depending on how it’s taken. A pill might need to be twice as strong as an injection to have the same effect.
Once in the blood, most drugs bind to proteins - especially albumin. About 95-98% of many drugs stick to these proteins and become inactive. Only the small free portion can interact with your cells. This is critical for safety. If another drug comes along and kicks your medicine off those proteins, suddenly too much free drug floods your system. Warfarin, a blood thinner, binds to proteins at 99%. If you take a sulfonamide antibiotic, it can displace warfarin, doubling your bleeding risk. That’s why pharmacists ask about every medication you’re on.
When Medications Are Safe to Use
Safety isn’t just about dosage. It’s about matching the right drug to the right person at the right time.
Lithium, used for bipolar disorder, has one of the narrowest safety margins of any drug. The difference between a helpful dose and a toxic one is tiny: 0.6 to 1.2 mmol/L in the blood. Too low, and mood swings return. Too high, and you risk tremors, confusion, kidney damage, or even seizures. That’s why regular blood tests aren’t optional - they’re life-saving.
Antibiotics like penicillin work by breaking down the walls of bacteria. They’re safe for humans because our cells don’t have those walls. But if you’re allergic, your immune system attacks the drug like a foreign invader. That’s why asking about allergies isn’t just routine - it’s essential.
Some drugs are safe only if you avoid certain foods. MAO inhibitors (used for depression) can cause dangerous spikes in blood pressure if you eat aged cheese, cured meats, or tap beer. These foods contain tyramine, which interacts with the drug. One ounce of blue cheese can have 1-5 mg of tyramine. A single serving might not seem like much - until it triggers a hypertensive crisis.
Even over-the-counter drugs carry risks. NSAIDs like ibuprofen can cause kidney damage in people with existing conditions, and acetaminophen can cause liver failure if taken in excess. The maximum daily dose isn’t just a suggestion - it’s a hard limit.
Why Understanding Your Medication Reduces Risk
Patients who understand how their drugs work are less likely to have bad reactions. A 2023 survey by the American Cancer Society found that 78% of patients on trastuzumab who knew how it targeted HER2 could identify early signs of heart damage - like shortness of breath or swelling - and reported them sooner. Those who didn’t understand the mechanism? Only 29% noticed.
On Reddit’s r/Pharmacy community, a top thread in 2023 showed how warfarin users learned to manage vitamin K. Leafy greens like kale and spinach contain 200-800 mcg of vitamin K per serving. Vitamin K counteracts warfarin. So if you suddenly eat a big salad every day, your blood won’t thin properly. But if you eat consistent amounts, your dose can be adjusted to match. Knowledge turns a scary drug into a manageable tool.
Statins, used to lower cholesterol, often cause muscle pain. But many people stop taking them because they don’t realize this pain is a warning sign - not just a side effect. When patients understand that statins block HMG-CoA reductase (the enzyme that makes cholesterol), they also learn that muscle damage can happen if the drug builds up. That’s why reporting muscle soreness early can prevent rhabdomyolysis - a rare but life-threatening breakdown of muscle tissue.
PatientsLikeMe data from 2023 showed that 68% of users worried about side effects. But 42% said they’d feel more confident if they understood their drug’s mechanism. Simple explanations - like "SSRIs work like putting a cork in the serotonin recycling tube" - help people connect symptoms to cause.
What Makes a Drug Risky?
Not all drugs are created equal in terms of safety. Some have well-defined targets. Others are like a sledgehammer in a china shop.
Statins are precise. They block one enzyme. You can monitor cholesterol levels to see if they’re working - and adjust the dose accordingly. That’s why they’re among the safest long-term medications.
Compare that to Dimebon, an antihistamine used in Russia for years. It showed promise in early Alzheimer’s trials, but later failed because scientists didn’t fully understand how it worked. Without knowing the mechanism, they couldn’t predict side effects or optimize dosing. It’s a classic case of hope without understanding.
The thalidomide disaster in the 1960s is another lesson. One version of the molecule helped with morning sickness. The other caused severe birth defects. They were mirror images - enantiomers - but the body treated them completely differently. Today, drug makers test each version separately. But many older drugs still have unclear mechanisms.
The FDA now requires detailed mechanism data for high-risk drugs. For example, natalizumab (Tysabri) reduces inflammation in multiple sclerosis by blocking immune cells from entering the brain. But that also raises the risk of a rare brain infection called PML. Doctors must complete training on this mechanism before prescribing it. That’s not bureaucracy - it’s protection.
What You Can Do to Stay Safe
- Ask your doctor or pharmacist: "How does this drug work?" Don’t settle for "it helps with X."
- Know your drug’s main side effect and what to watch for. For example, if you’re on warfarin, know the signs of bleeding: unusual bruising, pink urine, nosebleeds.
- Keep a list of all medications - including supplements. Many interactions happen with herbal products like St. John’s Wort or garlic pills.
- Don’t change doses without talking to your provider. Even small changes can be dangerous if the drug has a narrow therapeutic window.
- Use one pharmacy. They can flag dangerous combinations you might miss.
- Use apps or printed guides that explain your drug’s mechanism. Visuals help more than paragraphs.
Medicines are powerful. They save lives. But they also carry hidden risks. The best defense isn’t just following instructions - it’s understanding why those instructions exist.
Can I take two medicines if I don’t know how they interact?
No. Even over-the-counter drugs can interact dangerously. For example, taking ibuprofen with warfarin increases bleeding risk. Antihistamines with sedatives can cause extreme drowsiness. Always check with a pharmacist before combining medications - even if they seem harmless.
Why do some drugs need blood tests?
Drugs with narrow therapeutic indexes - like lithium, warfarin, or certain seizure medications - have a tiny gap between the right dose and the toxic dose. Blood tests measure how much drug is in your system. Without them, you could overdose without knowing. These aren’t optional checkups - they’re safety checkpoints.
Does it matter if I take my pill with food?
Yes. Some drugs need food to be absorbed properly - like certain antibiotics or antifungals. Others, like thyroid medication, must be taken on an empty stomach because food blocks absorption. Grapefruit juice can interfere with over 85 medications by blocking enzymes that break them down, causing dangerous buildup. Always follow the label or ask your pharmacist.
What if I feel fine - do I still need to take the medicine?
Some medications work silently. Blood pressure pills, statins, and antidepressants often don’t make you feel "better" right away - they prevent damage over time. Stopping them because you feel fine can lead to heart attacks, strokes, or relapse. The goal isn’t always to feel different - it’s to stay healthy.
Can natural supplements interfere with my prescription?
Absolutely. St. John’s Wort can reduce the effectiveness of birth control, antidepressants, and HIV drugs. Garlic and ginkgo can increase bleeding risk with blood thinners. Even vitamin K supplements can undo the effect of warfarin. Always tell your doctor what supplements you take - they’re not "harmless."
Why do some people have side effects and others don’t?
Genetics play a big role. About 28% of adverse drug reactions are linked to gene variations that affect how your body processes drugs. For example, some people metabolize codeine too quickly and get dangerous levels of morphine. Others process it too slowly and get no pain relief. Pharmacogenomic testing is becoming more common to match drugs to your biology.





