For many people, type 2 diabetes doesn’t come with a loud alarm. It creeps in quietly - a little more tired than usual, always thirsty, losing weight without trying, or noticing dark patches on the neck. By the time symptoms are obvious, the condition has often been growing for years. And here’s the hard truth: type 2 diabetes isn’t just about sugar. It’s about your body’s ability to use insulin, and when that system breaks down, it affects your heart, kidneys, nerves, eyes, and even your brain.
What Actually Happens in Type 2 Diabetes?
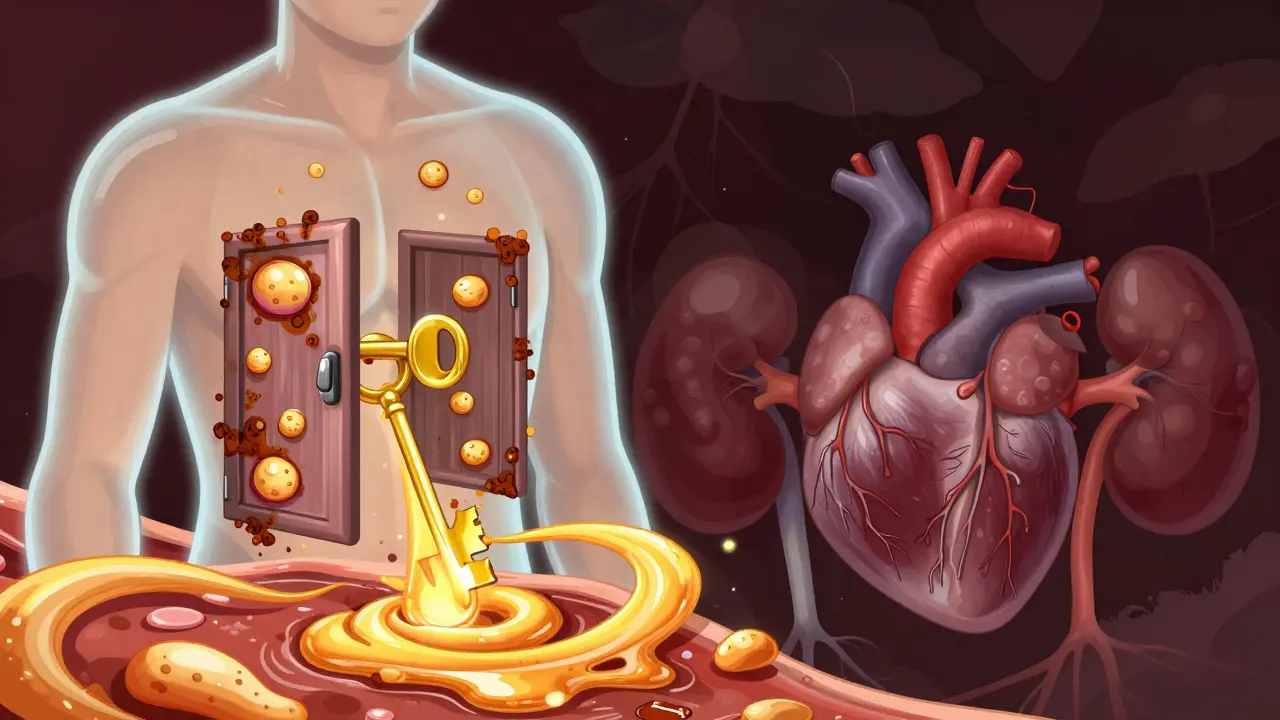
Type 2 diabetes isn’t caused by eating too much sugar alone. It’s a metabolic problem where your body’s cells stop responding properly to insulin - a hormone that acts like a key, unlocking cells so glucose (sugar) can enter and be used for energy. This is called insulin resistance. At first, your pancreas tries to compensate by pumping out more insulin - sometimes two or three times the normal amount. But over time, the pancreas wears out. Beta cells, which produce insulin, begin to die off. By the time most people are diagnosed, they’ve already lost about half of their insulin-making capacity.
This isn’t a sudden event. It’s a slow burn. And the triggers? They’re mostly lifestyle-based, but genetics play a big role too. If your parent or sibling has type 2 diabetes, your risk jumps by 40%. Certain ethnic groups - including African Americans, Hispanic/Latino, Native American, and Asian American populations - face higher rates. But the biggest driver? Weight. People with a BMI over 30 are 80 times more likely to develop it than those with a BMI under 22. And it’s not just about being overweight. Even a small amount of extra fat around the belly can throw your metabolism out of balance.
Signs You Might Have Type 2 Diabetes (Mostly Subtle)
Many people don’t realize they have type 2 diabetes until they’re already dealing with complications. That’s because symptoms often show up slowly. Here’s what actually happens in real life:
- You’re drinking more water than ever - not because it’s hot, but because your body is trying to flush out excess sugar through urine. That’s polydipsia - excessive thirst - and it affects 78% of newly diagnosed people.
- You’re peeing every hour, even at night. That’s polyuria, and it’s tied directly to the sugar pulling fluid out of your blood.
- You’re hungry all the time, even right after eating. Why? Because your cells aren’t getting the fuel they need. Sugar is in your blood, but it can’t get into your cells without insulin. That’s persistent hunger, reported by 65% of patients.
- You’ve lost weight without trying. Sounds odd, right? But when your body can’t use glucose for energy, it starts breaking down fat and muscle. That’s unexplained weight loss, seen in nearly half of cases.
- You’re constantly tired. Not just “I stayed up late” tired. Real, bone-deep fatigue. That’s because your cells are starved for energy. It affects 83% of people at diagnosis.
- Your vision gets blurry. High blood sugar swells the lenses in your eyes. This happens in over half of new cases.
- Cuts take forever to heal. Or you keep getting skin infections or urinary tract infections. That’s because high glucose weakens your immune system. One in three people with undiagnosed diabetes has recurring infections.
- Your feet tingle or go numb. That’s paresthesia, an early sign of nerve damage. It’s not just discomfort - it’s a warning that your nerves are being damaged by sugar.
- You notice dark, velvety patches on your neck, armpits, or groin. That’s acanthosis nigricans, a visible sign of insulin resistance. It’s found in up to half of people with prediabetes or early type 2.
And here’s the scary part: 15-20% of people with type 2 diabetes show no symptoms at all. They find out during a routine blood test - or after a heart attack.
Why You Can’t Just “Eat Less Sugar”
Most people think cutting out soda or candy will fix type 2 diabetes. It helps - but it’s not enough. The problem isn’t just sugar. It’s how your body handles all carbohydrates, and how your fat tissue, muscles, and liver respond (or don’t respond) to insulin.
Think of it like this: your body is a locked house. Insulin is the key. In type 2 diabetes, the locks get rusty. Even if you have plenty of keys (insulin), the doors won’t open. That’s insulin resistance. And it’s worsened by sitting too much. In fact, physical inactivity contributes to 27% of global type 2 diabetes cases. You don’t need to run marathons. Just moving more - walking after meals, taking the stairs, standing up every hour - can improve insulin sensitivity.
Genetics load the gun. Lifestyle pulls the trigger. If you have a family history, you’re not doomed. But you are at higher risk. And if you’re over 45, your risk climbs. But here’s something new: more than 287,000 Americans under 20 now have type 2 diabetes. It used to be called “adult-onset.” Now it’s hitting kids and teens - mostly because of rising obesity and sedentary lifestyles.

What Happens If You Don’t Manage It
Uncontrolled type 2 diabetes doesn’t just mean high blood sugar. It means damage - silent, slow, and serious.
- Heart disease: People with type 2 diabetes are 2 to 4 times more likely to have a heart attack or stroke. In fact, 65-80% of deaths among people with diabetes are from cardiovascular problems.
- Nerve damage (neuropathy): Affects 60-70% of people after 10 years. That tingling in your feet? It can turn into numbness. And numbness means you might not feel a blister - which can turn into a foot ulcer. One in five of those ulcers leads to amputation.
- Kidney failure: Type 2 diabetes causes 44% of all new cases of kidney failure requiring dialysis. Your kidneys filter waste - but too much sugar damages their tiny filters.
- Eye damage (retinopathy): 28.5% of adults with diabetes develop it. It’s the leading cause of new blindness in working-age adults in the U.S., with 17,000 cases every year.
- Mental health: Depression is twice as common in people with diabetes. And it’s not just sadness - it’s linked to a 20% higher risk of death. Managing diabetes is hard. It’s exhausting. And depression makes it harder.
- Brain health: There’s growing evidence linking type 2 diabetes to Alzheimer’s disease. Some researchers now call Alzheimer’s “type 3 diabetes” because brain cells become resistant to insulin too.
This isn’t fearmongering. It’s reality. But the good news? You can stop or delay most of this.
How to Manage Type 2 Diabetes - Real, Practical Steps
Management isn’t about perfection. It’s about consistency. Here’s what actually works, based on the latest guidelines from the American Diabetes Association (ADA) and real-world studies.
1. Lifestyle Changes - The Foundation
The CDC’s National Diabetes Prevention Program found that losing just 7% of your body weight through diet and exercise cuts your risk of developing diabetes by 58%. That’s not a magic number - it’s a threshold. For someone who weighs 200 pounds, that’s 14 pounds. Not 50. Not 100. 14.
What does that look like in practice?
- Swap sugary drinks for water, unsweetened tea, or sparkling water.
- Fill half your plate with non-starchy vegetables (broccoli, spinach, peppers, zucchini).
- Choose whole grains over white bread, rice, or pasta.
- Move for at least 30 minutes most days. Walk after dinner. Take the stairs. Park farther away. You don’t need a gym.
- Try to lose 5-10% of your body weight. Even that small loss improves insulin sensitivity.
2. Medications - When Lifestyle Isn’t Enough
Metformin is still the first-line drug. It’s cheap, safe, and reduces HbA1c by 1-2%. It doesn’t cause weight gain or low blood sugar. Most people tolerate it well - though some get stomach upset at first.
For people who need more help - especially those with heart or kidney disease - newer drugs are now preferred:
- GLP-1 receptor agonists (like semaglutide or liraglutide): These lower blood sugar and help you lose 3-5 kg. They also protect your heart.
- SGLT2 inhibitors (like empagliflozin or dapagliflozin): These make your kidneys flush out sugar through urine. They help your heart and kidneys, and cause 2-3 kg weight loss.
- Tirzepatide (Mounjaro): Approved in 2022, this dual-action drug lowers HbA1c by up to 2.3% and helps people lose 11-15 kg. It’s not for everyone, but it’s changing the game.
Insulin isn’t a failure. It’s a tool. If your pancreas stops making enough, insulin injections become necessary. That doesn’t mean you’ve “lost.” It means your body needs help.
3. Monitoring - Know Your Numbers
Most people check their blood sugar with a finger prick. But now, continuous glucose monitors (CGMs) are becoming more common - even for type 2. These small sensors track sugar levels all day, showing you how food, stress, or sleep affects you. In 2022, CGM use among Medicare beneficiaries jumped from 1.2% to 12.7% after insurance coverage expanded. That’s a game-changer.
Your HbA1c target? For most adults, it’s under 7%. But it’s personal. Younger, healthier people might aim for 6.5%. Older adults with other health problems might do better with a target of 7.5-8%. The goal isn’t perfection - it’s avoiding damage.
Can Type 2 Diabetes Be Reversed?
Yes - and not just “controlled.” Remission is possible. That means your HbA1c drops below 6.5% without medication.
The DIALECT trial in 2021 showed that 46% of people with type 2 diabetes for less than 6 years went into remission after a strict 850-calorie-per-day diet for 3-5 months, followed by gradual food reintroduction. That’s not starvation. It’s a medically supervised reset. And it works best early.
Weight loss is the key. The more weight you lose - especially belly fat - the more likely your pancreas can recover. Some people regain normal insulin function. Their bodies start working again.
But remission isn’t permanent. If you gain weight back, the diabetes can return. So it’s not a cure. It’s a reset. And it takes ongoing effort.
What’s Next? The Future of Type 2 Diabetes
Science is moving fast. Hybrid closed-loop systems (like the MiniMed 780G) now work for type 2 diabetes too. These devices automatically adjust insulin based on real-time glucose readings. They’re not perfect - but they improve time-in-range from 51% to 71%.
Meanwhile, research like the All of Us program is studying how genetics, environment, and social factors affect diabetes in different communities. Why do Native Americans have 14.5% prevalence? Why do some people lose weight easily and others don’t? Precision medicine is the next frontier.
But the biggest barrier isn’t science - it’s access. People without insurance, stable housing, or healthy food options struggle most. Technology won’t help if you can’t afford it.
Final Thought: You’re Not Broken
Type 2 diabetes isn’t your fault. It’s not because you’re lazy or weak. It’s a complex disease shaped by genes, environment, stress, sleep, and access to care. But you can take control - not by being perfect, but by being consistent. Small changes add up. Walking after dinner. Drinking water. Getting your HbA1c checked. Talking to your doctor about new medications. These aren’t chores. They’re acts of self-care.
The goal isn’t to be “cured.” It’s to live well - with energy, without pain, and without fear of what’s next.
Can type 2 diabetes be cured completely?
There’s no permanent cure for type 2 diabetes, but remission is possible. This means blood sugar levels return to normal without medication - usually after significant weight loss and lifestyle changes. The DIALECT trial showed that 46% of people with early-stage diabetes achieved remission after a structured low-calorie diet. But if weight is regained, diabetes can return. So while you can reverse symptoms, ongoing management is still needed.
Is type 2 diabetes only caused by eating too much sugar?
No. While sugary drinks and refined carbs contribute, the main driver is insulin resistance, often linked to excess belly fat, physical inactivity, and genetics. Even people who eat healthy can develop it if they have a strong family history or carry excess weight. Sugar alone doesn’t cause it - but it can worsen the problem.
Do I need to take insulin for life if I’m diagnosed with type 2 diabetes?
Not necessarily. Many people manage type 2 diabetes with diet, exercise, and oral medications like metformin. Insulin is usually added later - when the pancreas can’t make enough. Some people use insulin temporarily, especially after diagnosis or during illness. Others never need it. It depends on how much insulin your body still produces and how well you manage lifestyle factors.
Can I stop taking medication if I lose weight?
Yes - but only under medical supervision. Losing 5-10% of your body weight can improve insulin sensitivity enough to reduce or eliminate the need for medication. But stopping meds without checking your blood sugar first can be dangerous. Your doctor will guide you through gradual adjustments and monitor your HbA1c to ensure your levels stay in range.
How often should I check my blood sugar?
It depends. If you’re on insulin or certain medications, you may need to check daily. If you’re managing with lifestyle changes alone, checking once or twice a week might be enough. Continuous glucose monitors (CGMs) give real-time data and are becoming more common. Ask your doctor what’s right for you - there’s no one-size-fits-all answer.
What’s the best diet for type 2 diabetes?
There’s no single “best” diet. The most effective approach is one you can stick to. Low-carb, Mediterranean, plant-based, or calorie-controlled diets all work if they help you lose weight and improve insulin sensitivity. Focus on whole foods: vegetables, lean proteins, healthy fats, and fiber. Avoid processed carbs, sugary drinks, and excessive saturated fats. Portion control matters more than any specific food label.
Can stress or sleep affect my blood sugar?
Absolutely. Stress triggers hormones like cortisol that raise blood sugar. Poor sleep - especially under 6 hours a night - worsens insulin resistance. People with diabetes who sleep poorly often have higher HbA1c levels. Managing stress through mindfulness, exercise, or therapy - and prioritizing sleep - can have a bigger impact than you think.
Are there natural supplements that help with type 2 diabetes?
Some supplements like magnesium, chromium, or cinnamon show small benefits in studies - but none replace proven treatments. The American Diabetes Association doesn’t recommend supplements as primary therapy. They can interact with medications or have side effects. Always talk to your doctor before starting anything. Lifestyle and medication are still the most reliable tools.
Why do some people with type 2 diabetes need to take more than one medication?
Type 2 diabetes is a progressive disease. Over time, your body loses insulin-producing cells, and insulin resistance gets worse. One drug often isn’t enough. Combining medications - like metformin with a GLP-1 agonist - targets different parts of the problem: how your body uses insulin, how your liver releases sugar, and how your kidneys handle glucose. Multiple drugs can be safer and more effective than high doses of one.
Can type 2 diabetes be prevented if I have a family history?
Yes - even with a strong family history. The Diabetes Prevention Program showed that people at high risk reduced their chance of developing diabetes by 58% through 7% weight loss and 150 minutes of weekly exercise. Genetics load the gun, but lifestyle pulls the trigger. Prevention is possible, even likely, if you act early - before symptoms appear.






14 Comments