
Hormonal Imbalance Symptom Checker
Select symptoms you've experienced to identify possible hormonal imbalances affecting your cycle:
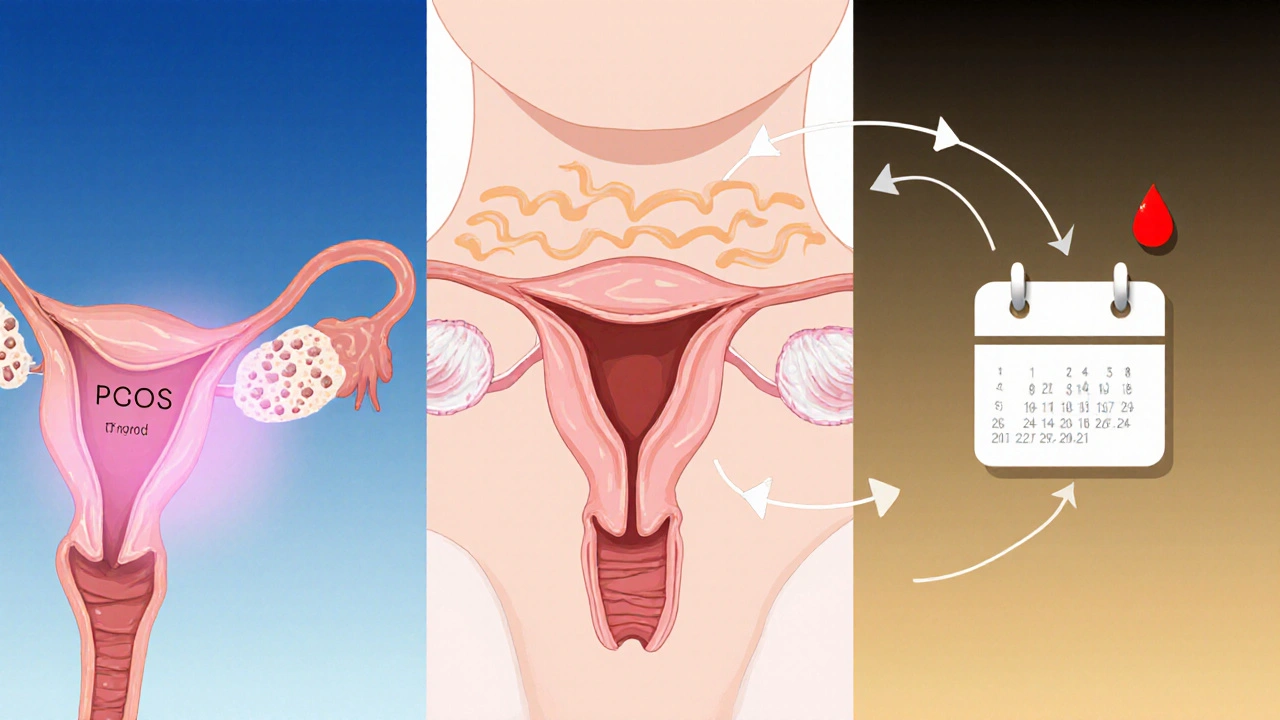
PCOS Irregular periods
Thyroid Weight changes
Prolactin Breast tenderness
Estrogen Heavy bleeding
Progesterone Spotting
FSH/LH Infertility
Possible Hormonal Imbalance Detected
If you're experiencing these symptoms regularly, consult with a healthcare provider for proper testing and diagnosis.
Hormonal imbalances affect ovulation and menstruation by disrupting the delicate feedback loops between the brain, ovaries, and other glands. Conditions like PCOS, thyroid disorders, and elevated prolactin can all cause irregular cycles, missed periods, or fertility issues.
Common indicators include irregular periods, unexplained weight changes, heavy bleeding, spotting, and difficulty conceiving.
Quick Take
- Hormonal imbalance can halt ovulation, cause missed periods, or lead to irregular cycles.
- Key players are estrogen, progesterone, FSH, LH, thyroid hormones, and prolactin.
- Conditions like PCOS, thyroid disease, and high prolactin levels are common culprits.
- Lifestyle tweaks (diet, sleep, stress management) often restore balance, but medication may be needed.
- Early diagnosis prevents long‑term fertility issues and improves overall health.
When the body’s chemistry goes off‑track, the whole monthly rhythm can wobble. Hormonal imbalance is a condition where the levels of one or more hormones deviate from their normal range, disrupting the feedback loops that control reproductive processes and many other systems. Understanding why this happens-and how it interferes with ovulation and menstruation-helps you spot warning signs and take action before fertility takes a hit.
Understanding Hormonal Balance
Reproductive health hinges on a tightly choreographed dance of hormones. Each hormone has a specific job, and the timing of its rise or fall tells the body what to do next.
Estrogen is the primary female sex hormone that promotes the growth of the uterine lining and prepares the body for egg release. It peaks in the first half of the cycle, signaling the brain to release a surge of LH.
Progesterone is produced after ovulation by the corpus luteum, it stabilizes the uterine lining for potential implantation. Low progesterone after ovulation often leads to spotting or early shedding.
The pituitary gland releases two gate‑keepers: Follicle‑stimulating hormone (FSH) is responsible for recruiting and maturing ovarian follicles during the early cycle and Luteinizing hormone (LH) is the trigger that causes the mature follicle to burst and release the egg (ovulation). A mis‑step in either hormone throws the whole schedule off.
Beyond the core reproductive hormones, the thyroid gland and the pituitary’s prolactin also play supporting roles. Thyroid hormones are critical for metabolism; too much or too little can slow or speed up the menstrual cycle. Prolactin is a hormone that primarily encourages milk production, but elevated levels can suppress FSH and LH, leading to anovulation.
How Hormones Drive Ovulation
The ovulatory phase is the climax of the first half of the menstrual cycle, often called the follicular phase. It unfolds in three steps:
- Follicle recruitment: Early in the cycle, FSH nudges several follicles to start growing. Usually only one reaches dominance.
- Estrogen surge: The dominant follicle secretes estrogen, which thickens the uterine lining and feeds back to the brain to prepare for the LH spike.
- LH surge and egg release: When estrogen hits a threshold, the hypothalamus releases a massive LH burst. This surge forces the follicle to rupture, releasing the egg-a process called ovulation.
If any of these steps falters, ovulation may not happen (anovulation). For example, low FSH means fewer follicles mature, while excess estrogen without a proper LH surge can keep the follicle stuck.
Menstrual Cycle Regulation
Once the egg is released, the luteal phase begins. The ruptured follicle transforms into the corpus luteum, which pumps out progesterone. Progesterone tells the uterine lining to stay thick, ready for implantation.
If fertilization doesn’t occur, the corpus luteum dies, progesterone drops, and the lining sheds-what we see as menstrual bleeding. This drop also resets the hypothalamic‑pituitary axis, readying the body for a new cycle.
When hormone levels are out of whack, this feedback loop breaks. Too much estrogen without adequate progesterone can cause a prolonged, heavy bleed (menorrhagia). Low progesterone can trigger early spotting, while erratic LH surges can lead to unpredictable cycle lengths.
Common Imbalances & Their Impact
Several medical conditions tip the hormonal scales. Below is a quick snapshot of the most frequent culprits.
| Hormone | Normal Role | Typical Imbalance | Result on Cycle |
|---|---|---|---|
| Estrogen | Builds uterine lining, promotes follicle growth | Excess (often in PCOS) or deficiency (menopause) | Heavy bleeding or skipped periods |
| Progesterone | Stabilizes lining post‑ovulation | Low after ovulation | Spotting, luteal phase defect |
| FSH | Stimulates follicle maturation | Low (hypothalamic dysfunction) or high (menopause) | Irregular or absent ovulation |
| LH | Triggers ovulation | Insufficient surge | Anovulation, infertility |
| Thyroid hormones | Sets metabolic pace, influences menstrual timing | Hypothyroidism or hyperthyroidism | Long or short cycles, amenorrhea |
| Prolactin | Promotes lactation | Hyperprolactinemia | Suppressed FSH/LH, missed periods |
Polycystic ovary syndrome (PCOS) is a hormonal disorder marked by excess androgens, insulin resistance, and often elevated estrogen without regular ovulation. Women with PCOS usually face irregular cycles, acne, and weight gain.
Thyroid disorders are another big player. Hypothyroidism is a condition where the thyroid produces too little hormone, slowing metabolism and often causing heavy, prolonged periods. Conversely, hyperthyroidism is an overactive thyroid that can quicken the cycle, leading to light or missed periods.
Elevated prolactin, sometimes triggered by stress, certain medications, or pituitary tumors, can shut down the LH surge. The result? Anovulation and potentially infertility.
Symptoms & When to Seek Help
Spotting a problem early makes treatment easier. Common red flags include:
- Missed periods for three or more consecutive months
- Cycles consistently shorter than 21 days or longer than 35 days
- Heavy bleeding that soaks a pad or tampon every hour
- Unexplained weight gain, acne, or excess facial hair
- Persistent mood swings, fatigue, or hair loss
If you notice any of these, a simple blood panel (FSH, LH, estradiol, progesterone, TSH, prolactin) can reveal the underlying imbalance. Ultrasound imaging helps confirm PCOS or structural issues.
Managing Hormonal Imbalance
Treatment blends lifestyle tweaks with medical interventions. Here’s a practical toolbox:
- Nutrition: Low‑glycemic diets curb insulin spikes, which can lower androgen excess in PCOS. Include whole grains, lean protein, and plenty of leafy greens.
- Exercise: Regular cardio and resistance training improve insulin sensitivity and can modestly raise progesterone levels.
- Stress reduction: Mindfulness, yoga, or even a consistent sleep schedule lower cortisol, which indirectly stabilizes LH and FSH.
- Supplement support: Vitamin D, magnesium, and omega‑3 fatty acids have shown modest benefits for menstrual regularity.
- Medication:
- Combined oral contraceptives (COCs) rebalance estrogen and progesterone, often restoring regular cycles.
- Metformin improves insulin resistance in PCOS, sometimes leading to spontaneous ovulation.
- Levothyroxine treats hypothyroidism, normalizing cycle length.
- Dopamine agonists (e.g., cabergoline) lower prolactin when hyperprolactinemia is the cause.
- Fertility‑focused drugs: Clomiphene citrate or letrozole can jump‑start the LH surge for women trying to conceive.
Regular follow‑up with a healthcare provider ensures doses stay appropriate and side effects are caught early.

Frequently Asked Questions
Can stress alone cause a missed period?
Yes. Chronic stress raises cortisol, which can blunt the hypothalamic release of GnRH, the signal that ultimately drives FSH and LH. When those pituitary hormones dip, ovulation may stop and periods become irregular.
Is it normal for estrogen to be higher than progesterone before ovulation?
Absolutely. The follicular phase is defined by a rising estrogen curve that prepares the endometrium and sets the stage for the LH surge. Progesterone stays low until after the egg is released.
How long does it take for thyroid medication to regularize periods?
Most people see a change within 6‑8 weeks of reaching a stable TSH level, but full cycle regularity may take a few additional months as the endometrial lining stabilizes.
Can I get pregnant with PCOS if I’m cycling irregularly?
Yes, many women with PCOS conceive naturally. The key is to induce at least one ovulation per cycle, often achieved with lifestyle changes, metformin, or ovulation‑inducing drugs.
What blood tests reveal the most about my menstrual health?
A comprehensive panel includes estradiol, progesterone, FSH, LH, prolactin, thyroid‑stimulating hormone (TSH), and sometimes androgens (testosterone, DHEA‑S) to spot PCOS‑related excess.
Understanding the hormonal orchestra behind your cycle empowers you to make informed choices. Whether the issue stems from a thyroid glitch, PCOS, or high prolactin, pinpointing the imbalance is the first step toward a steadier rhythm.






19 Comments
Wow, this tool is super useful! 🎉 Tracking those pesky symptoms is the first step to getting your cycle back on track. Keep logging everything, even the tiny changes – they add up fast!
Stay motivated and don’t forget to celebrate each little win along the way.
Let me add some clarity: the hypothalamic-pituitary-ovarian axis is a tight feedback loop, and any disruption – whether from PCOS, thyroid dysfunction, or hyperprolactinemia – can throw off both ovulation and menstruation.
It’s not just "feelings"; the hormone levels actually alter follicle development and endometrial shedding. Get proper labs and work with a specialist to map the exact imbalance.
Picture this: hormones as a volatile soap opera, each character vying for the spotlight, and the director (your brain) desperately trying to keep the plot coherent. When one actor decides to improvise, the whole drama collapses into chaos – missed periods, unexpected weight swings, endless frustration.
Yo, this checker is kinda rad! I jus’ love how it flags stuff quick n easy – no need 2 be a med student to get the gist. :) If ur noticing weird bleedin’ or weight flips, take note and hit up a doc pronto, k?
👍 Absolutely, keeping a log helps you see patterns that might otherwise slip by. When you notice a trend – say, spotting right after a stressful week – you can correlate it with lifestyle factors and discuss it intelligently with your provider. Keep it up! 🌟
Hormonal balance, when considered from a cross‑cultural perspective, reveals a tapestry of lived experiences that transcend the purely biochemical narrative; indeed, the perception of menstruation varies widely across societies, influencing how women interpret and respond to symptoms. In some Indigenous communities, for example, the menstrual cycle is celebrated as a rite of passage, and any deviation is addressed through communal rituals that aim to restore equilibrium. Conversely, in highly industrialized nations, the emphasis on productivity often leads to the medicalization of even minor irregularities, prompting a cascade of diagnostic tests and pharmaceutical interventions. This divergence underscores the importance of contextualizing hormonal data within the sociocultural framework of the individual. Moreover, the feedback loop involving the hypothalamus, pituitary gland, and ovaries is modulated not only by circulating estrogen and progesterone but also by psychosocial stressors, nutritional status, and circadian rhythms, each of which can differ starkly between cultures. Historical records from ancient Egypt show that women used herbal concoctions to regulate flow, a practice that parallels certain modern phytotherapy approaches. Similarly, traditional Chinese medicine attributes menstrual irregularities to imbalances in Qi and blood, prescribing acupuncture and dietary adjustments to harmonize the system. While the underlying endocrine physiology remains consistent – involving GnRH pulses, LH surges, and FSH‑driven folliculogenesis – the therapeutic lenses through which these processes are viewed are remarkably diverse. This multiplicity of perspectives invites clinicians to adopt a more holistic, patient‑centered approach, integrating biomedical diagnostics with respectful acknowledgment of cultural beliefs. By doing so, we can improve adherence to treatment plans, reduce the stigma associated with menstrual disorders, and ultimately empower women to take charge of their reproductive health. In conclusion, the interplay between hormonal imbalances and cultural context is not merely an academic curiosity; it is a vital component of effective, compassionate care that acknowledges the whole person, not just the endocrine numbers.
From a strictly analytical standpoint, the data presented herein suffers from an oversimplification of the endocrine feedback mechanisms. While the interactive checklist offers an accessible interface, it fails to delineate the nuanced interplay between peripheral conversion of androgens and central gonadotropin release. Moreover, the absence of quantitative thresholds renders any inferred diagnosis speculative at best. A rigorous approach would incorporate serum assays, dynamic hormone challenges, and longitudinal tracking to elucidate causality. In sum, the tool is pedagogically valuable but lacks the granularity requisite for clinical decision‑making.
Great tool, very helpful, concise, easy to use, encourages regular tracking, and gives quick insights.
Look, buddy, it's simple – if you see your periods playing hide‑and‑seek, get a thyroid panel and a quick hormone panel. Don't overthink, just act. Trust me, early action saves a lot of hassle later.
Hey there! Just wanted to say you’re doing a fantastic job by paying attention to these signals. A little tip: pairing this symptom checker with a simple food diary can uncover hidden patterns, like caffeine spikes or late‑night snacking, that might be nudging your hormones sideways. Keep it up, and don’t hesitate to share any surprising findings!
Hormones are the body's silent philosophers, constantly questioning why they must rise and fall.
Imagine your cycle as a wild kaleidoscope of colors-each hue representing a hormone dancing in perfect (or imperfect) sync. When the shades start to blur, it’s a sign to paint over the chaos with mindful habits and a dash of professional insight. Keep swapping those palettes, and you’ll rediscover the vibrant rhythm you deserve.
Get your labs done now.
Sure, getting labs is fine, but let’s not forget that lifestyle, stress, and diet often play a bigger role than a single blood draw. Sometimes the over‑medicalized route distracts from practical tweaks that can restore balance sooner.
It’s amazing how many people think hormones are something you either have or don’t have, when in reality they’re a dynamic system that reacts to everything we do. Taking a moment each day to note mood shifts, sleep quality, and even the food you ate can reveal patterns that your doctor might miss in a snapshot appointment. Also, remember that stress isn’t just “in your head”-it triggers cortisol, which directly suppresses the reproductive axis, leading to those dreaded missed periods. So, finding ways to unwind-whether it’s a short walk, a quick meditation, or even a funny meme-can be just as therapeutic as any medication. And if you’re already seeing a specialist, bring that symptom log with you; it turns a vague conversation into a concrete data‑driven discussion. Keep at it, stay curious, and don’t get discouraged by setbacks. Your body will thank you.
From an ontological perspective, the dysregulation of the hypothalamic‑pituitary‑gonadal axis can be conceptualized as a perturbation of the homeostatic set‑point within a complex adaptive system. The resultant phenotypic expression-be it oligomenorrhea, amenorrhea, or hypermenorrhea-reflects a cascade of feedback aberrations, wherein the neuroendocrine‐immune interface is compromised. Empirical quantification via serum estradiol, progestogen, and LH/FSH ratios, coupled with cortisol profiling, is indispensable for delineating etiological subtypes. Moreover, the integration of chronobiological data, such as melatonin secretion patterns, can elucidate circadian misalignment contributory to the pathology. In clinical praxis, a multimodal therapeutic regimen-encompassing selective estrogen receptor modulators, levothyroxine titration, and lifestyle optimization-should be calibrated to recalibrate the systemic equilibrium.
Interesting points. I’ve found that just taking a few minutes to breathe deeply while noting symptoms can actually lower stress hormones, which sometimes does the trick without any meds.
Great summary, thanks for the clear takeaways.
While the sentiment is appreciated, there are several grammatical inaccuracies in prior comments: "Hormones are the body's silent philosophers" should be "Hormones are the body's silent philosophers," with a comma; likewise, "gets" should be "gets," and "its" needs an apostrophe in "it's". Precision matters when discussing scientific topics.