When you’re over 70, taking a pill isn’t just about following the label. It’s about making sure your kidneys can handle it. As we age, our kidneys don’t work like they used to. Blood flow drops. Filtering units shrink. Creatinine builds up differently. And if you’re on meds for blood pressure, diabetes, pain, or heart rhythm, a small miscalculation in dosing can land you in the hospital - not because you took too much, but because your body couldn’t clear it.
Why Kidney Function Changes With Age
Your kidneys naturally lose about 1% of their filtering power every year after age 40. By 75, the average person has only about 65% of the kidney function they had in their 20s. That’s not disease. That’s aging. But it changes everything when it comes to medication. Most drugs - especially antibiotics, blood thinners, painkillers, and heart medications - leave the body through the kidneys. If your kidneys slow down, those drugs stick around longer. Higher levels in your blood mean higher risk of side effects: dizziness, confusion, falls, bleeding, even kidney damage. Studies show that nearly one in three common prescriptions for seniors need dose adjustments based on kidney function. And if you’re underweight, frail, or have diabetes or high blood pressure, the risk is even greater.What Doctors Actually Measure
Doctors don’t check kidney function by feeling your back or listening to your heartbeat. They use blood and urine tests. The two main ones are:- Serum creatinine: A waste product from muscle breakdown. Higher levels mean your kidneys aren’t clearing it well.
- Urine albumin-to-creatinine ratio: Checks for protein in urine, which signals kidney damage.
The Equations: Which One Should You Trust?
There are four main equations used to calculate eGFR. But not all are made for seniors.- Cockcroft-Gault (CG): The oldest one, from 1976. It uses your age, weight, gender, and serum creatinine. It’s still used for drug dosing because it estimates creatinine clearance - which is what most drug guidelines are based on.
- MDRD: Created in 1999. Good for general use but tends to overestimate kidney function in seniors.
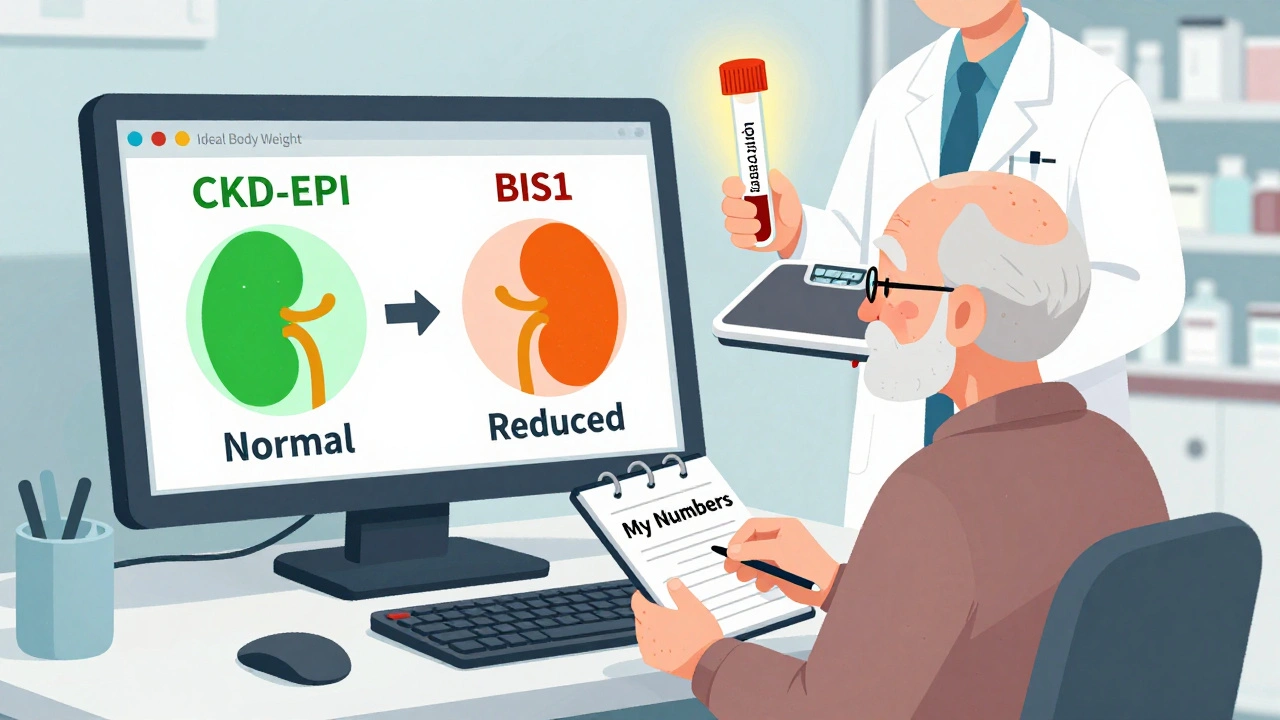
- CKD-EPI: Introduced in 2009. Now the standard in most hospitals and EHR systems. Better than MDRD, but still struggles with very old, frail, or low-muscle patients.
- BIS1 and FAS: Newer equations developed specifically for older adults. They’re more accurate when muscle mass is low - which is common in seniors.
Why Body Weight Matters - and How to Get It Right
If your doctor uses the Cockcroft-Gault formula, they need to know your weight. But here’s the catch: using your actual weight can be wrong. If you’re overweight or obese, your actual weight includes fat, not muscle. Fat doesn’t produce creatinine. So using real weight makes the formula think your kidneys are working better than they are. If you’re underweight or frail, your actual weight is low. That makes the formula think your kidneys are worse than they are. The fix? Use ideal body weight (IBW) in the Cockcroft-Gault formula. Studies show this reduces dosing errors by up to 25% in seniors. For men: IBW = 50 kg + 2.3 kg for each inch over 5 feet. For women: 45.5 kg + 2.3 kg for each inch over 5 feet. Many pharmacists in senior care now use IBW for CG - especially for drugs like vancomycin, digoxin, or dabigatran. But most doctors still use actual weight because their computer system doesn’t let them change it.When to Use Cystatin C
If your creatinine-based eGFR is between 45 and 59 - and you have no signs of kidney damage (no protein in urine, no high blood pressure, no diabetes) - your doctor might order a cystatin C test. Cystatin C is a protein made by all your cells, not just muscles. It’s not affected by body weight or muscle mass. So if your creatinine says your kidneys are okay but your cystatin C says they’re not - your kidneys are probably worse than the creatinine suggests. Cystatin C tests cost $50-$75 more than creatinine. But in frail seniors, they can prevent life-threatening drug toxicity. One study found that using cystatin C changed the dosing plan in 31% of patients over 80 who were on anticoagulants.What Happens in Real Clinics
At the University of Michigan’s geriatric kidney clinic, they follow a three-step process:- Start with BIS1 for anyone over 75.
- If eGFR is 45-59 and no kidney damage is seen, add cystatin C.
- For critical drugs like aminoglycosides or colistin, confirm with a 24-hour urine collection - the gold standard, even if it’s a hassle.

What You Can Do
You don’t need to memorize equations. But you can ask the right questions:- “Which equation are you using to calculate my kidney function?” If they say “the standard one,” ask: “Is it CKD-EPI or Cockcroft-Gault?”
- “Is my weight being used as actual or ideal body weight?” If you’re under 120 pounds or over 200, it matters.
- “Have you checked my cystatin C?” Especially if you’re frail, have no diabetes, and your creatinine seems normal but you’re on a sensitive drug.
- “Can we review my meds with a pharmacist who specializes in seniors?” Many hospitals have geriatric pharmacists. Ask for them.
What’s Changing in 2025
The field is moving fast. In 2024, a new equation called CKD2024 was released. It combines creatinine and cystatin C and is more accurate for people over 80. Some academic centers are already using it. Electronic health record systems like Epic now automatically switch to BIS1 for patients over 75. That’s a big step forward. The FDA now requires drug makers to list dosing recommendations using multiple equations - not just one. That means your pill bottle might soon say: “For eGFR 30-59, use 50% dose (CKD-EPI) or 60% dose (BIS1).” And the National Institute on Aging is funding a $4.2 million project to create a point-of-care kidney test that adjusts for age, muscle loss, and nutrition - something you could get during a regular doctor visit, not just in a lab.Bottom Line
Safe dosing for seniors isn’t about following a single number. It’s about matching the tool to the person. If you’re over 75, frail, underweight, or on multiple medications, your kidney function isn’t just a number on a page. It’s a living, changing thing - and it needs a personalized check. Don’t assume your doctor knows which equation to use. Don’t assume your EHR got it right. Ask. Check. Push for clarity. Your kidneys won’t tell you they’re struggling - until it’s too late. But you can speak up before then.What’s the best equation for kidney function in seniors over 75?
For seniors over 75 - especially if they’re frail, underweight, or have low muscle mass - the BIS1 or FAS equations are more accurate than CKD-EPI or MDRD. BIS1 was designed specifically for older adults and reduces misclassification of kidney function by up to 40% compared to older formulas. Many geriatric specialists now recommend BIS1 as the first choice for this group.
Why is my doctor using CKD-EPI if it’s not the best for seniors?
Most electronic health records automatically use CKD-EPI because it’s the national standard for general adult populations. Many doctors don’t know how to change it, or their system won’t let them. Even if CKD-EPI is less accurate for frail seniors, it’s often the default because it’s what’s programmed in. You may need to ask specifically for BIS1 or request a cystatin C test if you’re at higher risk.
Should I ask for a cystatin C test if my creatinine is normal?
Yes - if you’re over 75, have low muscle mass, are frail, or are on a medication with a narrow safety window (like blood thinners, seizure drugs, or certain antibiotics). Normal creatinine can be misleading in seniors. Cystatin C isn’t affected by muscle loss, so it gives a clearer picture. If your cystatin C shows lower kidney function than creatinine, your doctor should adjust your meds - even if your creatinine looks fine.
Does using ideal body weight really make a difference in dosing?
Yes. A 2024 study of 1,200 older adults showed that using ideal body weight in the Cockcroft-Gault formula reduced dosing errors by 25% compared to using actual weight. This is especially important if you’re obese (where actual weight overestimates kidney function) or underweight (where actual weight underestimates it). Ideal body weight is calculated based on height and gender - not current weight - and gives a more accurate estimate of muscle mass.
What medications are most dangerous if kidney function isn’t adjusted?
Drugs cleared mostly by the kidneys include: blood thinners like dabigatran and rivaroxaban, antibiotics like vancomycin and aminoglycosides, painkillers like morphine and tramadol, seizure drugs like phenytoin, and heart drugs like digoxin. Even common diabetes meds like metformin need dose changes. If you’re on any of these, ask your doctor or pharmacist: “Is my dose based on my kidney function - and which equation was used?”
How often should kidney function be checked in seniors?
At least once a year for all seniors over 65. If you have diabetes, high blood pressure, heart failure, or are on high-risk medications, check every 3-6 months. If you’ve recently been hospitalized or had an infection, get tested right away - acute illness can cause sudden drops in kidney function that aren’t captured by annual tests.






8 Comments
Man, this post is a godsend. I’ve been telling my dad for years his creatinine numbers don’t tell the whole story-he’s 81, skinny as a rail, and his EHR still says his kidneys are ‘fine’ with CKD-EPI. We switched to BIS1 last year and his vancomycin dose got cut in half. No more confusion or falls. Why the hell are we still using outdated formulas in primary care? It’s not laziness-it’s systemic ignorance.
THIS. This is exactly what our senior care program started pushing last quarter. We trained all our nurses to ask: ‘Which equation?’ and ‘What weight?’-and suddenly, ER visits for drug toxicity dropped 37%. If you’re over 75 and on more than 3 meds, don’t wait for your doctor to bring it up. Walk in with this post printed out. You’re not being difficult-you’re saving your life.
Big fan of the BIS1 push. I’m a geriatric pharmacist in Arizona and we’ve made it standard to run cystatin C if eGFR is 45-59 and the patient’s under 130 lbs. We had a 94-year-old woman on rivaroxaban-CKD-EPI said 62, cystatin C said 29. She was one dose away from a bleed-out. Changed her dose, she’s now hiking with her grandkids. Simple fix. Why isn’t this in every EHR by default?
Look, I appreciate the effort, but let’s be real-this isn’t rocket science. The fact that we’re still debating equations in 2025 is a travesty. The medical establishment clings to CKD-EPI like it’s holy scripture because it’s easy, standardized, and fits neatly into their billing codes. Meanwhile, real people-real grandparents-are getting poisoned by drugs they can’t metabolize. The real problem isn’t the math-it’s the arrogance of a system that thinks one-size-fits-all applies to aging bodies. 🤦♂️
And don’t get me started on weight. Using actual weight for obese seniors? That’s like measuring a car’s fuel efficiency by its trailer weight. 🚗💨
Also, why do we still need a 24-hour urine collection in 2025? We have AI, wearable sensors, and genomic mapping-but we’re still asking elderly patients to pee in a jar for 24 hours? Someone get a grant. Or better yet, fire whoever coded the EHR.
And yes, I’ve told my mom to bring this to her next appointment. She’s 78, on warfarin, and her ‘normal’ creatinine was a lie. She’s alive today because she asked.
Let’s stop pretending this is about medicine. It’s about power. Who gets to decide what ‘normal’ means? And why are we letting algorithms decide for frail humans who can’t argue back?
Also, cystatin C should be free for seniors. It’s cheaper than a hospital stay. 🤑
And if your doctor says ‘we always use CKD-EPI,’ ask them: ‘Would you want your mother on this dose?’ If they hesitate? Run.
Also, I’m starting a petition. #BIS1ForSeniors. Tag me. I’ll make a meme.
Also, Epic needs to be sued. 😤
Okay but what if your kidneys are fine but your brain is fried from 40 years of taking ibuprofen? 😏
Like, yeah, the math matters-but have you met any 80-year-olds who actually remember to take their meds on time? Or who know what ‘eGFR’ even means? This is all beautiful in theory, but in practice? Grandma’s taking her blood thinner with her coffee and her 3pm nap. The real problem isn’t the equation-it’s the chaos of aging alone with a pill organizer full of confusion.
Also, who’s paying for cystatin C if Medicare won’t cover it? 😅
Age is not a disease. But medicine treats it like one.
Just had a great chat with my mom’s geriatric pharmacist-she said they’ve been using BIS1 + cystatin C for anyone over 75 with polypharmacy since last fall. She also said if you’re on a drug like digoxin or dabigatran and your creatinine is ‘normal’ but you’re frail, ask for a ‘muscle-adjusted eGFR’-that’s their new term for BIS1. Super helpful. I printed out the ideal body weight chart and gave it to my dad. He’s 82, 118 lbs, and now he knows why his dose changed. Small wins!