
When your liver starts to fail, fluid doesn’t just pool in your legs-it builds up in your belly. That’s ascites. It’s not just uncomfortable; it’s a warning sign your liver is struggling. About half of people with cirrhosis will develop ascites within 10 years, and once it shows up, your chances of surviving two more years drop to 50%. The good news? You can manage it. The bad news? The advice you’ve heard might be wrong.
Why Fluid Builds Up in Your Belly
Ascites isn’t caused by drinking too much water. It’s caused by your liver getting damaged-usually from years of alcohol use, hepatitis, or fatty liver disease. When the liver scars, blood can’t flow through it easily. That raises pressure in the portal vein, the main blood vessel feeding the liver. This pressure pushes fluid out of your blood vessels and into your abdomen. But here’s the twist: your kidneys don’t help. Instead of flushing out salt and water, they hold onto it. Why? Because your body thinks you’re low on blood volume. It’s a trick your body plays on itself. The result? You retain more fluid than you lose. And the extra salt you eat? It makes it worse.Sodium Restriction: The Old Rule and the New Debate
For decades, doctors told patients with ascites to cut sodium to less than 2 grams a day. That’s about 5 grams of salt-roughly one teaspoon. It sounds simple. But try living on it. Most of the sodium in your diet doesn’t come from the salt shaker. It’s in bread, soup, canned veggies, deli meat, and even breakfast cereal. Cutting it to 2 grams means reading every label, avoiding restaurants, and cooking everything from scratch. Studies show fewer than 40% of patients can stick to that level. And now, new research is challenging the rule. Two major studies published between 2017 and 2022 found that people who ate 5 to 6.5 grams of salt a day (2-3 grams of sodium) had better outcomes than those on strict low-sodium diets. Their ascites improved more, they needed fewer fluid drains, and their kidneys stayed healthier. Why? Because going too low can backfire. When your body senses extreme salt deprivation, it tightens blood vessels in the kidneys. That reduces blood flow, which can trigger or worsen hepatorenal syndrome-a dangerous kidney failure that happens in advanced liver disease. One study showed the risk jumped from 18% to 35% in patients on ultra-strict diets. So what’s the truth? The experts aren’t sure. The American Association for the Study of Liver Diseases still recommends under 2 grams of sodium. But leading researchers like Dr. Pere Gines argue that strict restriction may do more harm than good. Dr. Frederick Wong from Toronto suggests a middle ground: aim for 5-6.5 grams of salt a day. Not zero. Not extreme. Just moderate.Diuretics: The Real Workhorses of Ascites Treatment
If sodium restriction alone doesn’t cut it-and it rarely does-diuretics are your next step. These are pills that help your kidneys flush out salt and water. Two drugs are used together: spironolactone and furosemide. Spironolactone is the first-line drug. It blocks a hormone that makes your body hold onto salt. Start with 100 mg a day. If you’re not losing fluid after 3 days, your doctor might bump it up by 100 mg every few days, up to 400 mg. It’s slow but steady. Furosemide is the faster-acting one. It’s added when spironolactone isn’t enough, usually for people who’ve had ascites before. Start at 40 mg a day, max out at 160 mg. The combo works because they hit different parts of the kidney. The goal? Lose no more than 0.5 kg (1 pound) a day if you don’t have swollen legs. If you do have edema, you can aim for up to 1 kg a day. Lose weight too fast, and you risk kidney damage or electrolyte crashes. You’ll need blood tests every few days at first. Your sodium, potassium, and kidney numbers will be watched closely. Too much diuretic can drop your sodium too low. That’s called hyponatremia. It happens in 30-40% of ascites patients. If your sodium falls below 130, your doctor will adjust your fluids and meds-not just add more diuretics.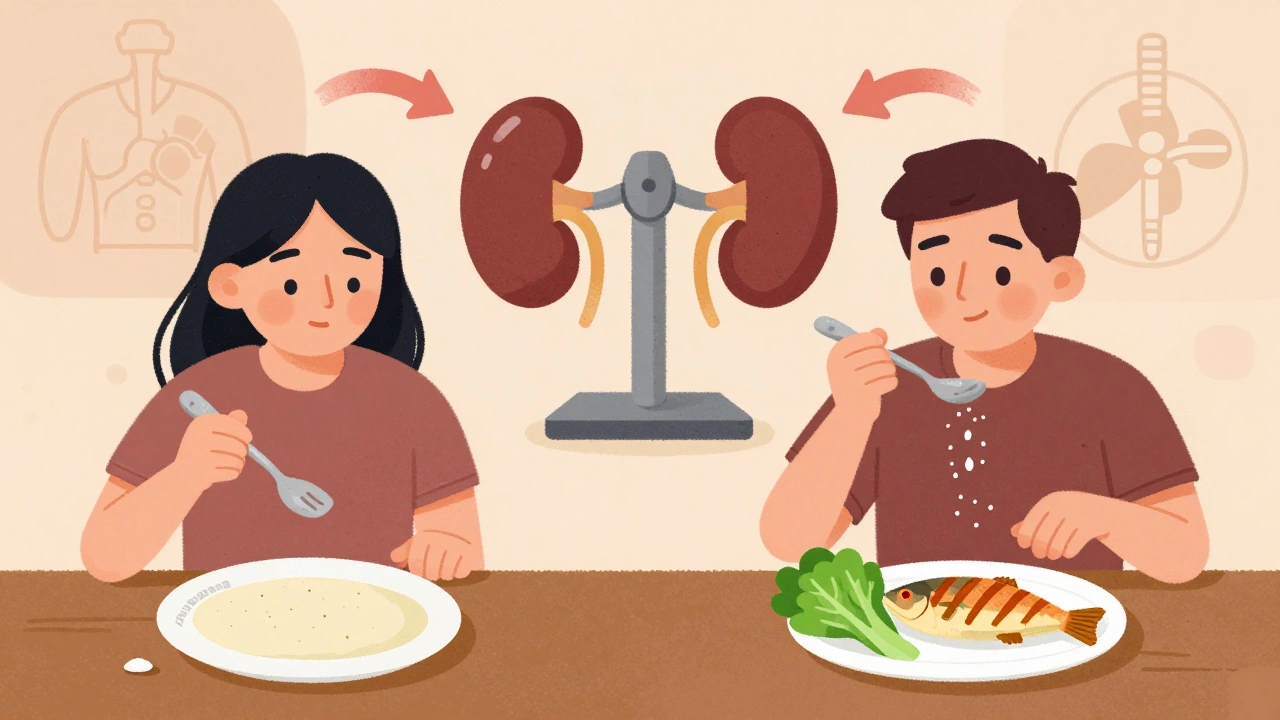
What Not to Take
Some common medications can make ascites worse. Avoid NSAIDs like ibuprofen or naproxen. They reduce blood flow to your kidneys, which can trigger kidney failure. ACE inhibitors and ARBs-used for high blood pressure-are also risky. One study found cirrhotic patients on these drugs had more than double the risk of ending up on dialysis. Even over-the-counter painkillers can be dangerous. If you need pain relief, talk to your doctor. Acetaminophen (Tylenol) is usually safer, but even that has limits in advanced liver disease.What If Diuretics Don’t Work?
About 5-10% of people with ascites don’t respond to maximum doses of diuretics. That’s called refractory ascites. It’s serious. Survival drops to about 50% within six months. The go-to fix? Large-volume paracentesis. That’s when a needle drains 5-10 liters of fluid from your belly in one session. It gives instant relief. But you can’t do it every week. Your body loses protein and albumin. That’s why you get an IV of human albumin-8 grams for every liter removed. It helps keep your blood pressure stable and protects your kidneys. This isn’t a cure. It’s a bridge. You’ll still need diuretics and diet changes. But for many, it’s the only way to feel normal again.What About New Drugs Like Vaptans?
There are drugs called vaptans-like tolvaptan-that block water retention. They sound perfect. But they’re expensive: $5,000 to $7,000 for a month’s supply. And you can only use them for 30 days at a time. They’re also risky if you’re already low on sodium. Most doctors save them for rare cases where everything else has failed.
Living With Ascites: Practical Tips
You don’t have to become a nutritionist. But you do need to make smart choices:- Choose fresh meat, fish, and vegetables over packaged or processed foods.
- Don’t add salt when cooking. Use herbs, lemon, or vinegar instead.
- Check labels. If a food has more than 200 mg of sodium per serving, skip it.
- Drink water normally-there’s no need to restrict fluids unless your sodium is very low.
- Weigh yourself every morning. A sudden 1 kg gain in a day means fluid is building up.
- Keep a food diary. It helps your doctor see if you’re eating more salt than you think.
The Big Picture: Personalized Care Is the Future
The old one-size-fits-all approach to sodium is fading. Doctors now look at your whole picture: How’s your kidney function? Are you malnourished? Can you even follow a strict diet? Some patients do better with moderate restriction. Others need the old 2-gram rule. A major trial called PROMETHEUS is underway and will release results in late 2025. It’s comparing unrestricted diets to strict ones in hundreds of patients. That could finally settle the debate. Until then, the best advice is simple: work with your doctor. Don’t assume you need to starve yourself of salt. Don’t assume diuretics alone will fix everything. And don’t ignore the signs-sudden weight gain, tight clothes, swelling in your legs-those mean it’s time to check in.When to Call Your Doctor
Call right away if you notice:- Abdominal pain or fever-could be infection in the fluid (spontaneous bacterial peritonitis).
- Confusion or drowsiness-signs of hepatic encephalopathy.
- Less urine output or yellowing skin-signs your kidneys or liver are failing.
- Weight gain of more than 1 kg in 2 days.
Ascites isn’t a death sentence. But it’s a signal. Your liver is telling you it needs help. The right mix of diet, medication, and monitoring can keep you out of the hospital and feeling better for longer.
Can I eat salt at all if I have ascites?
Yes, but in moderation. Strict salt restriction (under 2 grams of sodium daily) is no longer the universal rule. Recent studies show that moderate restriction-around 5 to 6.5 grams of salt per day (2-3 grams sodium)-may be safer and just as effective, especially when combined with diuretics. Avoid processed foods, and don’t add salt at the table.
How long does it take for diuretics to work on ascites?
Spironolactone usually starts working in 2-3 days, but it takes up to a week to reach full effect. Furosemide works faster-within hours. Most people see noticeable fluid loss in 5-7 days. Weight loss should be slow: no more than 0.5-1 kg per day to avoid kidney damage.
Why do I need to check my sodium levels so often?
Diuretics and sodium restriction can cause your blood sodium to drop too low (hyponatremia), which happens in up to 40% of ascites patients. Low sodium can cause confusion, seizures, or coma. Checking every few days at first helps your doctor adjust your meds before it gets dangerous.
Can I drink alcohol with ascites?
No. Alcohol continues to damage your liver, even if you’re on diuretics. Stopping alcohol is the single most important step you can take to slow liver disease and improve your chances of surviving ascites. Even small amounts can undo the benefits of treatment.
Is ascites reversible?
In early stages, yes-if the underlying liver damage is mild and you stick to treatment. Fluid can go down with diet, diuretics, and stopping alcohol. But if cirrhosis is advanced, ascites usually returns. That’s when treatments like paracentesis or liver transplant become necessary.
What foods should I avoid with ascites?
Avoid processed foods: canned soups, frozen meals, deli meats, pickles, soy sauce, chips, and breads with added salt. Also skip restaurant food unless you ask for no salt. Choose fresh fruits, vegetables, lean meats, and plain rice or pasta. Cook with herbs, garlic, lemon, or vinegar instead of salt.
Can I exercise with ascites?
Yes, but gently. Light walking, stretching, or seated exercises help circulation and prevent muscle loss. Avoid heavy lifting or intense workouts, which can raise pressure in your abdomen. Always check with your doctor first, especially if you’ve had recent fluid drains.




12 Comments