When your knee, shoulder, or hip suddenly locks up with sharp, burning pain-especially after a flare-up of arthritis or tendonitis-you’ve probably heard about corticosteroid injections. Also called cortisone shots, these are among the most common treatments for joint inflammation. But they’re not magic. They don’t fix damaged cartilage. They don’t cure arthritis. And if you get them too often, they might actually make things worse.
How Corticosteroid Injections Work
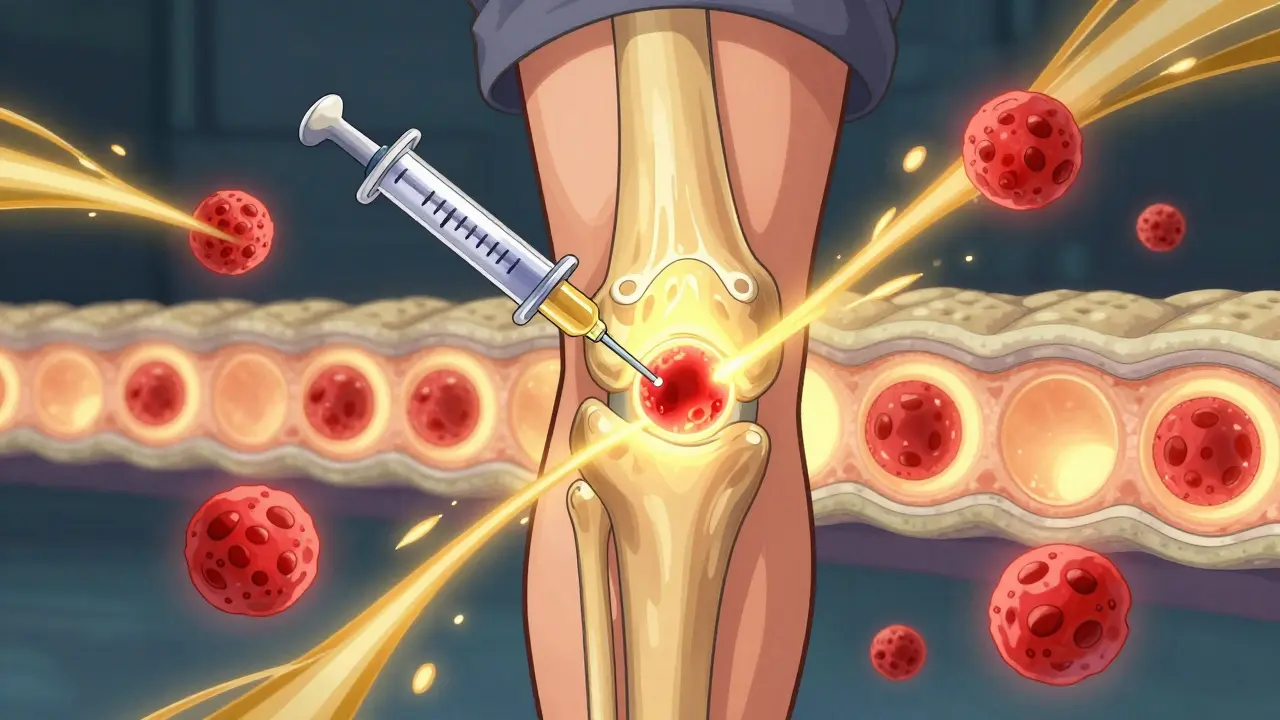
Corticosteroid injections deliver powerful anti-inflammatory drugs directly into the joint or around a sore tendon. The most common ones are triamcinolone acetonide, methylprednisolone acetate, and betamethasone. These aren’t the same as the steroids athletes abuse to build muscle. These are synthetic versions of cortisol, a hormone your body naturally makes to control inflammation.
Once injected, the drug enters the synovial fluid-the slippery liquid that cushions your joints. It shuts down the inflammatory cascade. Specifically, it blocks signals from cells that release chemicals like interleukin-1 and tumor necrosis factor-alpha, which cause swelling, heat, and pain. It also reduces the number of white blood cells in the joint and thickens the fluid slightly, which helps with cushioning.
Many injections mix the corticosteroid with a local anesthetic like lidocaine. You’ll feel immediate relief from the numbing agent-but that fades in a few hours. The real effect from the steroid kicks in 24 to 72 hours later. That’s when the swelling drops, the pressure eases, and the pain starts to fade.
Who Benefits Most?
These injections work best for inflammatory conditions, not structural damage. If your pain comes from:
- Acute gout flares
- Tennis elbow (lateral epicondylitis)
- Shoulder bursitis
- Rheumatoid arthritis flare-ups
- Tendonitis in the wrist or ankle
then a cortisone shot can be a game-changer. Many people report feeling like their old selves within days. One patient from the Arthritis Foundation community got back to playing competitive golf just 10 days after a hip injection.
But if your pain is from advanced osteoarthritis-where the cartilage is worn down, bones are grinding, and bone spurs have formed-corticosteroids won’t fix that. They might dull the pain temporarily, but they don’t repair tissue. In fact, repeated use in these cases can speed up joint breakdown.
How Long Does It Last?
Don’t expect permanent relief. On average, the pain reduction lasts 2 to 4 weeks. For some, it’s 6 to 12 weeks. Rarely, someone gets relief for 6 months. But studies show that after 6 weeks, the benefit fades to near baseline. At 24 weeks, there’s no difference between those who got the shot and those who got a placebo.
One major 2023 meta-analysis of 15 studies found that while corticosteroid injections beat saline (saltwater) shots in the first month, the gap disappeared after that. Another study showed that for lateral epicondylitis, cortisone gave better results than PRP or saline at 1 month-but by 3 months, all groups were about the same.
And here’s the catch: the more often you get them, the less they work. Many patients report diminishing returns. One Reddit user shared: “The first two knee injections gave me 8 weeks each. The third? Only 3 weeks-and a 3-day flare afterward.” That’s not rare. About 41% of users say the relief doesn’t last beyond 4 to 6 weeks.
Cost and Accessibility
Without insurance, a single corticosteroid injection costs between $100 and $300. That’s far cheaper than alternatives:
- Viscosupplementation (hyaluronic acid): $500-$1,000
- PRP (platelet-rich plasma): $500-$1,500
- Stem cell therapy: $2,000+
That’s why they’re still the go-to for many doctors. In 2022, over 10 million corticosteroid injections were given in the U.S. alone. They’re used in 15% of all orthopedic office visits. Primary care doctors are getting trained to give them too-32 U.S. states now allow it under expanded scope-of-practice rules.
There’s also a newer option: Zilretta, an extended-release form of triamcinolone approved by the FDA in 2023. It’s designed for osteoarthritis and can provide relief for up to 12 weeks in about 45% of patients-nearly double the duration of standard shots.
When They Don’t Work-or Make Things Worse
Corticosteroids are powerful, but they come with risks. The most common side effect is a post-injection flare. About 2-8% of people get a sudden spike in pain and swelling within 24-48 hours after the shot. It’s caused by the crystals in the steroid irritating the joint. Ice, rest, and over-the-counter NSAIDs usually fix it within a few days.
Other risks include:
- Temporary spike in blood sugar-especially dangerous for diabetics. Monitor glucose for 72 hours after the injection.
- Skin thinning or lightening at the injection site. This happens in about 17% of patients who get repeated shots in the same spot.
- Tendon weakening or rupture. This is rare, but it’s why doctors limit injections to every 3-4 months.
- Accelerated joint degeneration. A 2023 study found patients who got repeated knee injections had over 3 times higher odds of visible cartilage loss on X-rays.
And here’s a critical warning: if you’re planning joint replacement surgery, avoid cortisone shots within 3 months before. A 2023 study showed patients who had injections before knee or hip replacement had more than twice the risk of post-surgery infection.
How Many Is Too Many?
Most guidelines agree: no more than 3 to 4 injections per joint per year. The American College of Rheumatology updated its 2024 guidelines to strongly advise against repeated injections in joints with advanced osteoarthritis. The reasoning? There’s no evidence they help long-term-and clear evidence they can hurt.
Doctors often use the injection as a diagnostic tool too. If your pain disappears after a shot in the shoulder, it confirms the shoulder is the source-not your neck or heart. That’s why some orthopedists say it’s worth trying-even if it’s not a long-term fix.
What to Do After the Shot
Don’t rush back to the gym or heavy lifting. For the first 48 hours after the injection:
- Avoid strenuous activity
- Apply ice if you feel swelling
- Keep the area clean and dry
- Watch for signs of infection: redness, warmth, pus, fever
- If you’re diabetic, check your blood sugar 2-3 times a day for 3 days
Ultrasound guidance is now the gold standard. Studies show it increases injection accuracy from 70% to 95%. That means less risk of hitting the wrong spot and more consistent results. If your doctor doesn’t use ultrasound, ask why.
Alternatives to Consider
If you’ve had a few shots and the relief is fading, or you’re worried about long-term damage, here are other options:
- Physical therapy: Builds strength and movement patterns that reduce joint stress. Often more effective long-term than repeated injections.
- PRP (platelet-rich plasma): Uses your own blood to trigger healing. More expensive, but may help with tendon repair and early osteoarthritis.
- Weight management: Losing just 10 pounds reduces knee osteoarthritis pain by 50% in many cases.
- Bracing or orthotics: Can offload pressure from damaged joints.
- Low-impact exercise: Swimming, cycling, and walking keep joints moving without grinding them down.
Some clinics are now combining corticosteroids with PRP to get the quick relief of steroids and the healing potential of PRP. There are 27 active clinical trials testing this right now.
The Bottom Line
Corticosteroid injections are not a cure. They’re a tool. A very useful one-for short-term relief of inflammation. They work fast, they’re affordable, and they’re backed by decades of research. But they’re not meant to be a permanent solution.
If you’re getting them every few months, it’s a red flag. You’re masking symptoms, not fixing the problem. The real goal should be to use the injection as a window of opportunity-to get moving, start physical therapy, lose weight, or adjust your activity level-so you don’t need another shot next time.
Used wisely, they can give you back weeks or months of pain-free life. Used carelessly, they can speed up joint damage and leave you with fewer options down the road.
Do corticosteroid injections cure joint problems?
No. Corticosteroid injections reduce inflammation and pain temporarily, but they don’t repair damaged cartilage, heal tendons, or stop the progression of arthritis. They treat symptoms, not the root cause.
How soon after a cortisone shot will I feel better?
You’ll feel immediate numbness from the local anesthetic, but that wears off in a few hours. The steroid itself takes 24 to 72 hours to start working. Most people notice significant relief by day 3.
Can I get cortisone shots every month?
No. Most medical guidelines recommend no more than 3 to 4 injections per joint per year. More frequent use increases the risk of tendon rupture, cartilage damage, and infection. The body’s natural repair processes get suppressed over time.
Are cortisone shots safe for people with diabetes?
They can be, but with caution. Corticosteroids can cause a sharp rise in blood sugar for up to 72 hours after the injection. Diabetic patients should monitor glucose levels closely during that time and adjust insulin or medication as needed under their doctor’s guidance.
Is ultrasound guidance necessary for joint injections?
It’s not always required, but it’s strongly recommended. Ultrasound increases accuracy from about 70% to 95%, meaning the medication goes exactly where it’s needed. This improves results and reduces the risk of damaging nearby tissues like tendons or nerves.
What should I avoid after a cortisone injection?
Avoid heavy lifting, running, or high-impact activity for at least 48 hours. Don’t soak in hot tubs or saunas right away-heat can increase swelling. If you’re diabetic, avoid skipping meals or alcohol, which can interfere with blood sugar control.
Can cortisone shots cause weight gain?
Not from a single injection. Weight gain is a side effect of long-term oral steroid use, not localized joint injections. The dose used in a joint shot is very small and doesn’t enter the bloodstream in significant amounts to affect metabolism.
Do cortisone shots work for back pain?
Yes, but only for specific types. Epidural steroid injections can help with nerve-related back pain from herniated discs or spinal stenosis. They’re not used for general lower back pain from muscle strain or degenerative disc disease without nerve involvement.
Next Steps if You’re Considering an Injection
If you’re thinking about a corticosteroid injection, ask yourself:
- Is my pain from inflammation or from structural damage?
- Have I tried physical therapy or activity modification first?
- How many injections have I had in this joint over the past year?
- Do I have diabetes or a history of tendon injuries?
- Am I planning surgery in the next 6 months?
If you answered yes to any of the last three, talk to your doctor about alternatives. Use the injection as a bridge-not a crutch. The goal isn’t to avoid pain forever. It’s to move better, live fuller, and protect your joints for the long haul.






9 Comments
cortisone shots are just another way rich ppl pay to avoid real treatment. in nigeria we use herbs and prayer and still walk better than these folks with their fancy injections. the body dont need synthetic cortisol. its weak. they got weak joints because they sit all day and eat fast food. fix your lifestyle not your injection schedule.
Let me be perfectly clear-this entire post is dangerously incomplete without a deeper discussion of the epigenetic and systemic immunomodulatory consequences of repeated intra-articular corticosteroid administration. The 2023 meta-analysis cited? It’s underpowered. The real issue isn’t just cartilage loss-it’s the downregulation of collagen type II synthesis in chondrocytes mediated by glucocorticoid receptor signaling pathways, which occurs even at subclinical doses. And yet, primary care physicians are now being trained to administer these? That’s not medical progress-it’s systemic dereliction of duty. We’ve replaced clinical judgment with procedural convenience. The fact that Zilretta is even on the market is a testament to pharmaceutical innovation being driven by profit margins, not patient outcomes. If you’re getting more than two injections per joint annually, you’re not being treated-you’re being exploited.
Been there. Got three knee shots over two years. First one? Magic. Second? Meh. Third? Felt like someone kicked me in the knee with a steel toe boot for three days straight. Now I just ride my bike and do squats with a chair. No doctor, no shot, no drama. Also, why does everyone act like PRP is some miracle cure? I paid $1200 for it and felt nothing. Just a fancy blood draw with a side of hope.
ok but like… i got a cortisone shot last month for my wrist and i swear it was a 10/10. felt like my hand was reborn. i could finally hold my coffee cup again without crying. also my doc used ultrasound and it was SO much less scary than i thought. i’m not saying it’s forever but… for now? yes. 🙌
thank you for writing this. i’ve been scared to get one because i heard they ruin your joints… but now i feel like i get it. it’s not the shot that’s bad-it’s using it as a crutch. i’ve been doing PT for 6 months and finally got the shot last week. it’s not a cure, but it gave me the window to actually move again. 🌱
sooo… you’re telling me I paid $250 for a 3-week pain vacation and now my joint is crumbling? and my doc didn’t even use ultrasound? and i’m diabetic?? and now i’m supposed to just ‘do PT’?? like… where’s the time?? i work two jobs and my kid has soccer practice. this isn’t a wellness blog, this is survival. why does everything have to be so complicated? i just want to pick up my groceries without screaming.
I’ve seen patients who got 12 shots in one knee over five years. By the time they came to me, the joint was bone-on-bone. I didn’t blame them. They were just trying to live. But we need better systems-better access to PT, better insurance coverage for non-invasive options. The problem isn’t the patients. It’s the system that makes cortisone the easiest answer.
Just wanted to say-this is the most balanced, clear breakdown I’ve read. I’m a physical therapist and I see so many people stuck in the ‘shot cycle.’ The moment they get relief, they go right back to the same movement patterns that hurt them. The shot isn’t the enemy. The lack of follow-through is. Keep encouraging people to use the window. That’s the real win.