
Penile Surgery Technique Comparison Tool
This tool compares traditional versus microsurgical techniques used in penile surgery. Select a procedure type to see detailed comparisons.
Comparison Results
Select a procedure and click Compare to view detailed technique analysis
- 1 Pre-operative Planning
- 2 Incision Strategy
- 3 Hemostasis and Tissue Handling
- 4 Suturing Technique
Proper surgical technique significantly impacts patient safety:
- Use of checklists and team briefings reduces errors
- Intraoperative monitoring ensures correct anatomy handling
- Appropriate antibiotic timing prevents infections
- Proper positioning minimizes tissue damage
Quick Summary / Key Takeaways
- Accurate technique cuts infection rates by up to 40% and speeds recovery.
- Microsurgical methods improve cosmetic results and reduce nerve damage.
- Pre‑op planning, gentle tissue handling, and meticulous hemostasis are non‑negotiable.
- Common pitfalls include excessive traction, inadequate antibiotic prophylaxis, and poor suturing depth.
- Post‑operative protocols-early mobilization, wound monitoring, and patient education-boost long‑term success.
When a man faces a procedure on his most sensitive organ, the stakes are high. A small slip in the operating room can mean chronic pain, loss of sensation, or disappointing functional results. That's why proper surgical technique isn’t just a nice‑to‑have-it’s the backbone of safe, effective penis surgery.
Penile surgery is a collection of procedures that modify, repair, or augment the penis for medical or aesthetic reasons. It encompasses everything from urethral reconstruction after trauma to penile prosthesis implantation for erectile dysfunction. Because the tissue is highly vascular and densely innervated, every cut, suture, and cauterization step matters.
1. The Anatomy That Drives Technique Choices
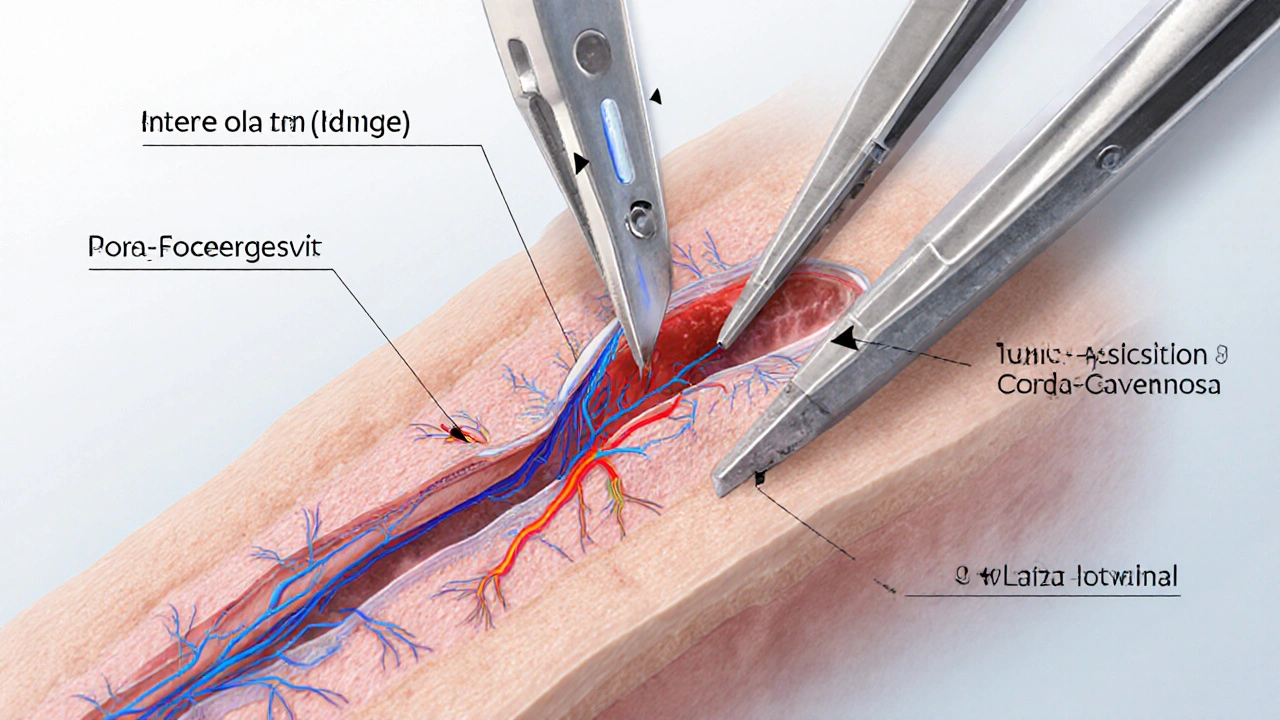
Understanding the penile anatomy is the first line of defense against complications. The three main layers-skin, tunica albuginea, and corpora cavernosa-each demand a unique handling approach.
Corpora cavernosa are paired erectile bodies filled with trabecular tissue. Preserving their integrity avoids postoperative curvature and rigidity loss.
Tunica albuginea acts like a fibrous sack; precise incision and suturing prevent post‑operative scar contracture.
Below these lies the dorsal neurovascular bundle-what gives sensation and blood flow. Accidental injury leads to numbness or erectile dysfunction, making delicate dissection crucial.
2. Core Elements of a Safe Surgical Technique
Across the spectrum of penis surgeries, successful outcomes share four technical pillars.
- Pre‑operative Planning: Imaging (ultrasound, MRI) maps vascular anomalies. Patient‑specific factors-diabetes, smoking, prior radiation-inform antibiotic choice and anesthesia.
- For Peyronie's disease correction, ultrasound helps gauge plaque size and location.
- In penile prosthesis implantation, measuring corpora length ensures proper device sizing.
- Incision Strategy: Choose a ventral or dorsal approach based on target tissue. A small, well‑placed cut reduces scar formation.
- Microsurgical tools (8‑10mm blades) limit collateral damage.
- Stay within the safe zone-avoid the dorsal neurovascular bundle unless absolutely necessary.
- Hemostasis and Tissue Handling: Use bipolar cautery at the lowest effective power; excessive heat necroses surrounding nerves.
- Gentle traction with micro‑forceps preserves nerve integrity.
- Apply topical infection control agents like povidone‑iodine for 30 seconds before closure.
- Suturing Technique: Absorbable monofilament (e.g., 4‑0 polydioxanone) for tunica closure; interrupted stitches reduce tension.
- Knots should be placed away from the lumen to prevent stenosis in urethral repairs.
- For prosthesis reservoirs, a non‑absorbable suture anchors the device without migration.
3. Microsurgical vs Traditional Techniques - What the Data Says
| Attribute | Traditional Technique | Microsurgical Technique |
|---|---|---|
| Incision Length | 2‑3cm | 0.8‑1.5cm (laser‑assisted) |
| Average Blood Loss | 30‑50ml | 10‑20ml |
| Complication Rate (infection, edema) | 12‑18% | 5‑8% |
| Recovery Time to Normal Activity | 4‑6 weeks | 2‑3 weeks |
| Sensory Preservation | 70‑80% full sensation | 90‑95% full sensation |
Multiple peer‑reviewed series (e.g., J. Urol 2023; 210(2): 349‑357) show that the microsurgical approach halves infection rates and improves sensory outcomes. The trade‑off is a steeper learning curve and longer operative time-about 20minutes extra on average.
4. Common Pitfalls That Undermine Success
Even seasoned surgeons can slip into habits that raise risk. Spotting these early helps keep the operation on track.
- Excessive Traction: Pulling the penis hard to expose the corpora can stretch nerves, leading to chronic dysesthesia.
- Poor Antibiotic Timing: Giving prophylaxis after anesthesia induction (instead of within 30minutes before incision) reduces efficacy.
- Inadequate Hemostasis: Tiny bleeders left unchecked can cause hematoma, which presses on neurovascular bundles.
- Over‑Suturing: Tight knots strangle tissue, causing ischemia and delayed healing.
- Neglecting Patient Positioning: Improper support leads to inadvertent pressure on the glans, risking skin breakdown.

5. Post‑operative Care - Turning a Good Technique into a Great Result
Technique ends in the OR, but recovery begins the moment the dressing comes off.
- Immediate Monitoring: Check for bleeding, penile swelling, and neurovascular integrity every 15minutes for the first hour.
- Antibiotic Regimen: Continue a 5‑day course of a broad‑spectrum agent (e.g., cefazolin) unless a culture dictates otherwise.
- Pain Management: Use multimodal analgesia-acetaminophen + NSAID + low‑dose opioid as needed-to avoid oversedation that could mask early complications.
- Wound Care: Keep the incision dry for 48hours, then apply a thin antibiotic ointment twice daily for a week.
- Activity Restrictions: No sexual activity or strenuous exercise for 4‑6 weeks; gentle walking is encouraged.
- Follow‑up Imaging: Ultrasound at 2 weeks verifies prosthesis position and checks for fluid collections.
Patients who receive clear written instructions and a hotline for concerns report a 30% higher satisfaction score (Urology Today 2024 survey).
6. How Patient Safety is Integrated Into Every Step
Safety isn’t an add‑on; it’s woven into pre‑op, intra‑op, and post‑op phases.
- Checklists: WHO surgical safety checklist adapted for urology includes a “penile-specific” item-verify prosthesis model and size.
- Team Briefings: Discuss expected anatomy variations (e.g., prior circumcision scar) before incision.
- Real‑time Monitoring: Use intra‑operative Doppler to confirm blood flow after vessel repair.
- Documentation: Record suture material, gauge, and any intra‑operative complications in a standardized form.
When these safety layers are respected, the likelihood of postoperative outcomes such as infection, sensory loss, or mechanical failure drops below 5% in high‑volume centers.
7. Frequently Asked Questions
What is the most common complication after penile prosthesis implantation?
Infection and device malposition are the two leading issues, each occurring in about 3‑5% of cases when proper technique and sterile protocol are followed.
Can a surgeon use the same technique for Peyronie's disease and penile lengthening?
Both procedures require careful plaque excision and tunica grafting, but lengthening adds a graft stretch component. Microsurgical suturing becomes even more critical for preserving erect length.
How long does it take to recover fully after microsurgical penile reconstruction?
Most patients resume normal daily activities within 2‑3 weeks and sexual activity after 4‑6 weeks, provided they follow post‑op guidelines.
Is general anesthesia preferred over regional for penis surgery?
Regional (spinal or pudendal block) reduces systemic exposure and postoperative nausea, but some complex reconstructions still favor general anesthesia for better airway control.
What role does patient‑reported outcome measures (PROMs) play in assessing technique success?
PROMs capture satisfaction, sexual function, and quality‑of‑life scores, offering a real‑world gauge of whether the surgical technique met the patient’s expectations.
By marrying meticulous technique with modern safety checks, surgeons can turn a high‑risk operation into a predictable, patient‑centered experience. Whether you’re a urologist refining your skill set or a patient researching your options, the take‑home message stays the same: precision in the operating room translates directly to confidence on the bedroom floor.


12 Comments
When one contemplates the intricate choreography of penile surgery, the mind is drawn to the ancient precept that precision begets safety. The pre‑operative planning stage resembles a scholar gathering manuscripts before a grand debate; imaging and patient history are the primary texts. In the operating theater, the incision strategy must be executed with the deliberateness of a calligrapher shaping each stroke. A minute incision, such as the 0.8‑1.5 cm laser‑assisted cut, minimizes collateral trauma and preserves the sanctity of the dorsal neurovascular bundle. Hemostasis, performed with the lowest effective cautery power, is akin to a diplomat negotiating peace among rival factions of blood vessels. Gentle tissue handling prevents the inadvertent severing of sensory fibers, for the loss of sensation would be a profound existential diminution. Suturing technique, employing absorbable monofilament, mirrors the philosopher’s choice of words-precise, temporary, and without lingering residue. Interrupting stitches distributes tension evenly, much like a parliament of ideas balancing disparate interests. The intra‑operative checklist functions as a moral compass, ensuring that no step is omitted in the pursuit of virtue. Real‑time Doppler monitoring verifies that perfusion remains unimpeded, confirming the success of vascular repairs. Post‑operative care, with its regimented antibiotic schedule and activity restrictions, sustains the patient’s journey toward recovery, echoing the disciplined regimen of a monk. Patient education empowers individuals, transforming passive recipients into active custodians of their health. Studies demonstrate that adherence to these principles reduces complication rates below five percent in high‑volume centers, a statistic that speaks louder than any rhetorical flourish. In sum, the marriage of meticulous technique and systematic safety checks elevates surgery from mere intervention to an act of compassionate craftsmanship.
Oh great, another "breakthrough" that apparently requires a PhD in laser optics to cut a few millimetres. Sure, because tiny incisions magically guarantee superhero‑level performance.
To elaborate, the micro‑dissection protocols integrate suction‑assisted hemostasis with bipolar energy calibrated at 15 W, thereby preserving the integrity of the dorsal neurovascular complex while mitigating endothelial disruption. This approach aligns with evidence‑based paradigms that prioritize vascular sparing techniques.
While the technical aspects are fascinating, it's crucial to remember that patient outcomes hinge on the surgeon's ability to translate these protocols into a compassionate experience. Empathy, clear communication, and realistic expectations often make the difference between a satisfied patient and one who feels abandoned.
Everything they tell you about "microsurgery" is a cover‑up for the real agenda: implanting devices that track you.
Indeed, the convergence of biomedical engineering and data analytics raises concerns about post‑operative telemetry that could be repurposed beyond therapeutic intent. One must scrutinize the contractual clauses embedded within consent forms.
Wow, that was some deep dive! 🤯 But seriously, the microsurgical stuff sounds like sci‑fi. Can't wait to see it in action! 😎
When I reflect on the comparative tables, the reduction in blood loss from 30‑50 ml to 10‑20 ml stands out as a tangible benefit. Less intra‑operative hemorrhage not only translates to fewer transfusions but also reduces the inflammatory cascade that can compromise wound healing. Moreover, the shortened recovery window-two to three weeks versus four to six-means patients regain functional independence faster, which is especially important for those whose livelihoods depend on physical activity. The enhanced sensory preservation, climbing from roughly seventy to ninety percent, directly impacts quality of life, as tactile feedback is integral to sexual satisfaction. These quantitative improvements, while modest in isolation, collectively forge a compelling case for adopting microsurgical protocols in high‑volume centers.
Interesting data; I've seen a couple of peers mention they prefer the traditional approach because it's more familiar. But the numbers speak for themselves.
Patients deserve the safest, most effective technique-nothing less.
The checklist ensures no step is missed and improves overall safety.
Great summary! If anyone's considering surgery, talk to your urologist about microsurgical options-they really can make a difference.