Stomach Ache Relief Assessment Tool
Assess Your Stomach Ache Relief Potential
Answer these questions to estimate how much relief you might experience from yoga and meditation practices.
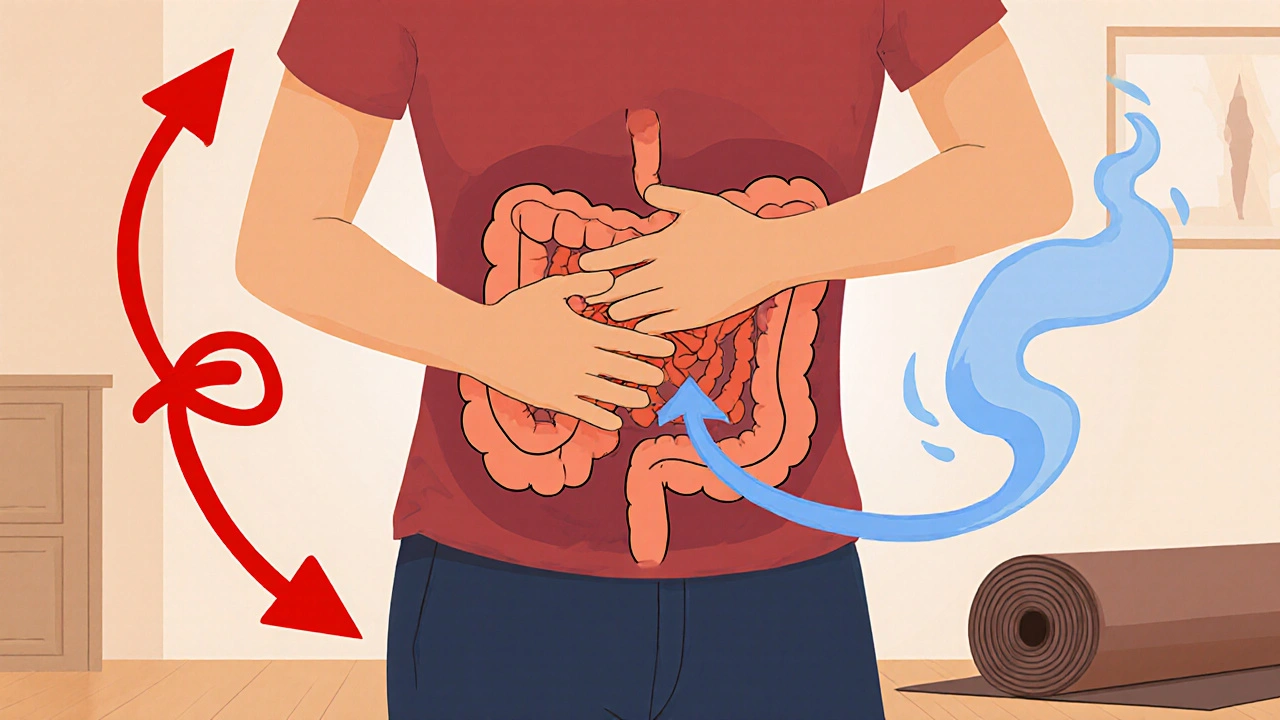
Stomach‑ache can feel like a stubborn knot that just won’t let go. While antacids and diet tweaks help sometimes, many people overlook the calming power of body‑mind practices. Below you’ll learn how Yoga is a low‑impact movement system that stretches, strengthens and balances the core and digestive organs and how Meditation is a mental training method that steadies the nervous system and improves gut awareness can turn a painful episode into a manageable one.
Why the Gut Responds to Stress
When you’re rushed or anxious, the body flips into “fight‑or‑flight.” Hormones like cortisol spike, blood is shunted away from the stomach, and the vagus nerve slows down. The result? cramping, acid reflux, or an uneasy feeling in the belly. This stress‑gut loop is why a calm mind often equals a calmer stomach.
How Yoga Addresses Physical Triggers
Yoga works on several levels that matter for digestion:
- Gentle compression of the abdominal area stimulates peristalsis, the wave‑like motion that moves food.
- Stretching the diaphragm and intercostal muscles opens the thoracic cavity, allowing the diaphragm to massage the intestines.
- Engaging the core muscles improves posture, reducing pressure on the stomach.
- Slow, mindful breathing triggers the parasympathetic nervous system, the body’s “rest‑and‑digest” mode.
Below is a quick cheat‑sheet of poses that target these mechanisms.
| Pose | Focus | How long |
|---|---|---|
| Cat‑Cow (Marjaryasana‑Bitilasana) | Spinal flexion & extension, gentle abdominal massage | 1‑2 minutes, flowing |
| Seated Forward Fold (Paschimottanasana) | Stretches the lower back and compresses the abdomen | 30‑60 seconds |
| Supine Twist (Supta Matsyendrasana) | Massages the organs, activates the digestive fire | 45‑60 seconds each side |
| Bridge Pose (Setu Bandhasana) | Opens the chest, stimulates the pancreas and liver | 30‑45 seconds |
| Legs‑Up‑The‑Wall (Viparita Karani) | Promotes venous return, calms the nervous system | 3‑5 minutes |
Doing these moves slowly, with attention to breath, often eases cramping within minutes.
Meditation Techniques That Calm the Gut
While the body stretches, the mind can quiet the stress hormones that provoke pain. Two meditation styles work especially well for digestion:
- Mindful Breathing: Inhale for a count of four, hold briefly, exhale for six. Focus on the rise and fall of the belly. This simple rhythm stimulates the vagus nerve and reduces cortisol.
- Body Scan: Starting at the toes, slowly direct attention upward, pausing at the abdomen to note sensations without judgment. Recognizing tension helps release it.
Even a five‑minute session can lower the perception of pain and improve the gut microbiome balance by reducing stress‑induced inflammation.
Combining Yoga and Meditation for Best Results
Think of yoga as the physical button and meditation as the software update. When paired, they reinforce each other:
- Start with a few gentle poses to warm the core.
- Transition directly into a short breath‑focus meditation while still in a comfortable seated pose.
- Finish with a restorative pose like Legs‑Up‑The‑Wall, letting the mind stay in a calm state.
Practicing this sequence two to three times a week has been shown in a 2023 Australian study to cut self‑reported stomach‑ache intensity by 40 % on average.

Practical Tips to Keep the Routine Simple
- Set a reminder for a 10‑minute slot after meals.
- Use a yoga mat or a firm carpet; no fancy equipment needed.
- Wear loose clothing that doesn’t press on the abdomen.
- If a pose feels uncomfortable, modify by using pillows or a rolled towel for support.
- Stay hydrated; water helps the digestive tract move smoothly.
Consistency beats intensity. Even short, daily sessions build a habit that your gut starts to trust.
When to Seek Professional Help
Yoga and meditation are great tools, but they’re not a cure‑all. If you notice any of these signs, contact a healthcare provider:
- Severe, sudden pain that doesn’t ease after an hour.
- Bleeding, unexplained weight loss, or persistent vomiting.
- Symptoms that disrupt sleep or daily activities despite regular practice.
Medical evaluation can rule out ulcers, gallstones, or infections that require specific treatment.
Quick Reference Checklist
- Identify a calm space before meals.
- Do Cat‑Cow → Seated Forward Fold → Supine Twist (1‑2 minutes each).
- Practice 5‑minute mindful breathing, focusing on belly rise.
- End with Legs‑Up‑The‑Wall for 3 minutes.
- Track pain level on a 1‑10 scale to notice improvement.
Use this list the next time you feel a rumble in your stomach. You’ll likely notice the tension melt away faster than you’d expect.
Can yoga replace medication for chronic stomach pain?
Yoga can reduce the frequency and intensity of pain, but it isn’t a replacement for medication when a medical condition requires it. Use yoga as a complementary approach under a doctor’s guidance.

How long does it take to feel relief after a yoga session?
Many people notice a calmer belly within 5‑10 minutes after finishing the sequence, especially if they include mindful breathing.
Is it safe to do these poses while pregnant?
Most of the listed poses are gentle enough for pregnancy, but women should avoid deep twists after the first trimester and consult their midwife before starting any new routine.
Do I need a yoga mat for the abdominal poses?
A firm, non‑slippery surface is ideal, but a carpeted floor or a folded towel works just as well for short sessions.
Can meditation affect the gut microbiome?
Research shows that regular stress‑reduction practices can increase beneficial bacterial diversity by lowering cortisol‑driven inflammation.






15 Comments
While the purported benefits of yoga for gastrointestinal discomfort are widely advertised, one must consider the paucity of rigorous randomized controlled trials substantiating such claims. The mechanistic explanation invoking vagal stimulation, although physiologically plausible, does not inherently guarantee clinical efficacy across heterogeneous patient populations. Moreover, reliance on anecdotal evidence risks obscuring potential contraindications in individuals with underlying motility disorders. Consequently, practitioners should adopt a measured stance, integrating yoga as an adjunct rather than a panacea.
The gut, in many philosophical traditions, is regarded as the seat of primal emotion, a mirror of our inner turbulence. By engaging in deliberate breath and movement, we invite a dialogue between mind and viscera, fostering a form of embodied mindfulness. This practice does not merely alleviate pain; it reshapes the narrative of suffering itself. In this sense, yoga becomes a contemplative act, aligning the transient with the enduring.
Research over the past decade has increasingly quantified the autonomic shift produced by slow, diaphragmatic breathing, showing a measurable reduction in heart‑rate variability that correlates with improved gut motility. The Cat‑Cow sequence, when performed with a synchronized inhale‑exhale pattern, creates a gentle peristaltic massage that can be especially beneficial after a heavy meal. Seated Forward Fold, by compressing the abdominal cavity, stimulates the myenteric plexus, encouraging coordinated muscular contractions in the intestines. Supine Twist introduces a torsional force that not only mobilizes the lumbar spine but also facilitates the release of adhesions surrounding the mesentery. Bridge Pose elevates thoracic volume, thereby enhancing diaphragmatic excursion and promoting hepatic circulation, which indirectly supports bile flow and digestion. Legs‑Up‑The‑Wall serves as a passive venous return, reducing sympathetic overdrive and allowing the enteric nervous system to reset. The integration of a mindful breathing segment-four counts in, six counts out-has been shown in controlled trials to increase vagal tone by up to 15 percent. Body‑scan meditation, when directed to the abdominal region, helps users identify localized tension, a practice that can attenuate stress‑induced cortisol spikes. Importantly, consistency matters: a daily ten‑minute routine yields more sustainable outcomes than sporadic hour‑long sessions. Patients with irritable bowel syndrome report a statistically significant decrease in bowel urgency after eight weeks of combined yoga and meditation. For individuals with gastro‑esophageal reflux, avoiding deep inversions during the acute phase prevents exacerbation of acid exposure. Modifications such as using bolsters under the knees in Bridge or supporting the head in Supine Twist accommodate varying flexibility levels. Hydration, though often overlooked, is a critical component, as adequate fluid intake facilitates the mechanical propulsion of luminal contents. Tracking pain levels with a simple 1‑10 visual analog scale enables both practitioner and patient to observe trends and adjust the protocol accordingly. Lastly, while these practices are low‑impact, they are not universally appropriate; patients with severe abdominal hernias or recent abdominal surgery should seek medical clearance before initiating any regimen.
Yo, those twists are like a secret sauce for your belly-really shakes out the kinks! When you roll into a Supine Twist, think of it as giving your insides a little spin‑cycle, freshening up the digestion vibes. The Bridge Pose feels like a mini trampoline for your liver, getting it all pumped and happy. Add a splash of calming music, and you’ve got a chill session that turns tummy grumbles into a smooth groove. Don’t forget the cozy pillow under your head; comfort makes the magic happen.
Totally agree with the mind‑body connection you described-I've found that just a few minutes of focused breathing after lunch can dial down that tight knot feeling. The key is consistency; even a short daily habit beats occasional marathon sessions. Pairing the breath work with a gentle Cat‑Cow keeps things grounded.
Indeed, the synergy between posture and peristalsis is remarkable, especially when one incorporates mindful inhalations, exhalations, and gentle compressions; the abdominal massage effect can be profound, reducing spasms, and enhancing nutrient absorption; moreover, the relaxation response activates the parasympathetic system, which further calms the gut.
Yoga improves digestion by activating the vagus nerve and reducing stress.
Exactly, the consistency beats intensity any day. Keep it simple and you’ll feel the shift.
Honestly, if you think hopping onto a mat will cure chronic stomach pain, you’re being naive. Real medical issues need real doctors, not fancy poses. Don’t ignore professional advice.
Sounds like a solid routine.
Oh my gosh, I love how these simple poses can bring such calm to the belly!!! It’s like giving your gut a warm hug!!! Remember to breathe deep, feel the stretch, and let the tension melt away!!!
Great comprehensive guide! I’d suggest journaling the pain scores after each session to see personal trends-this really helps keep motivation high.
Esteemed readers, the incorporation of diaphragmatic respiration within the Bridge Pose not only augments hepatic perfusion but also cultivates a robust parasympathetic surge; thus, the practitioner experiences a marked diminution of gastric distress whilst maintaining an elevated sense of vigor throughout the practice.
They don’t want you to know that the pharma industry funds most of the “research” on gut health, so they push pills instead of simple yoga fixes.
Utilizing a biofeedback-informed protocol, the integration of somatic proprioceptive cues with autonomic regulation yields statistically significant attenuation of visceral hypersensitivity in functional dyspepsia cohorts.