
Fluoroquinolone + NSAID Risk Calculator
Risk Assessment Tool
Calculate your combined risk of kidney and neurologic complications when taking fluoroquinolone antibiotics with NSAIDs. This tool helps evaluate whether these medications should be avoided together based on your specific health factors.
When you hear the words fluoroquinolone NSAID interaction, you might picture a lab report, not a real person dealing with pain and infection. In practice, the combo of a fluoroquinolone antibiotic and a non‑steroidal anti‑inflammatory drug (NSAID) can turn a short course of therapy into a long‑term health headache. This article breaks down why those two drug families clash, what the numbers say about kidney and brain risks, and how doctors and patients can stay safe.
What are fluoroquinolone antibiotics?
Fluoroquinolone antibiotics is a class of broad‑spectrum antimicrobial agents that includes ciprofloxacin, levofloxacin, moxifloxacin, norfloxacin and ofloxacin. First launched in the 1960s (nalidixic acid was the prototype), they quickly became the go‑to for urinary‑tract infections (UTIs), community‑acquired pneumonia, and many other bacterial ailments.
Regulators worldwide have flagged them for serious side‑effects. Health Canada’s 2017 safety review warned that tendon, nerve and central‑nervous‑system problems could be long‑lasting. The European Medicines Agency (EMA) logged 286 disabling reactions over 21 years, prompting stricter prescribing rules in the UK and across the EU.
What are NSAIDs?
NSAIDs cover drugs like ibuprofen, naproxen, diclofenac and celecoxib. They relieve pain, reduce fever, and tame inflammation by blocking cyclo‑oxygenase (COX) enzymes, the same pathway that creates protective prostaglandins in the stomach and kidneys.
While widely available over the counter, NSAIDs can also cause trouble-headaches, dizziness, and, in rare cases, aseptic meningitis. Their biggest safety concern is kidney injury, especially when the kidneys are already working at half‑capacity.
Why the two don’t mix: overlapping renal risks
The kidneys filter both fluoroquinolones and NSAIDs. When they’re taken together, the burden doubles. A 2013 study (PMCID PMC3708027) found that men on fluoroquinolones had a two‑fold rise in acute kidney injury (AKI) requiring hospitalisation. NSAIDs independently cut renal blood flow by reducing prostaglandin synthesis.
When the British National Formulary (BNF) notes that “nephrotoxic agents like fluoroquinolones and NSAIDs create additive risk,” it’s not just theory. JAMA Internal Medicine (2013; 173 (19): 1806‑1814) reported up to a 3.5‑fold increase in AKI among elderly patients taking both drug classes.
Mechanistically, fluoroquinolones can trigger acute interstitial nephritis, granulomatous inflammation, crystal formation when urine pH > 6.8, and even acute tubular necrosis. NSAIDs worsen the picture by shrinking the glomerular filtration rate-especially in volume‑depleted or already‑impaired kidneys.
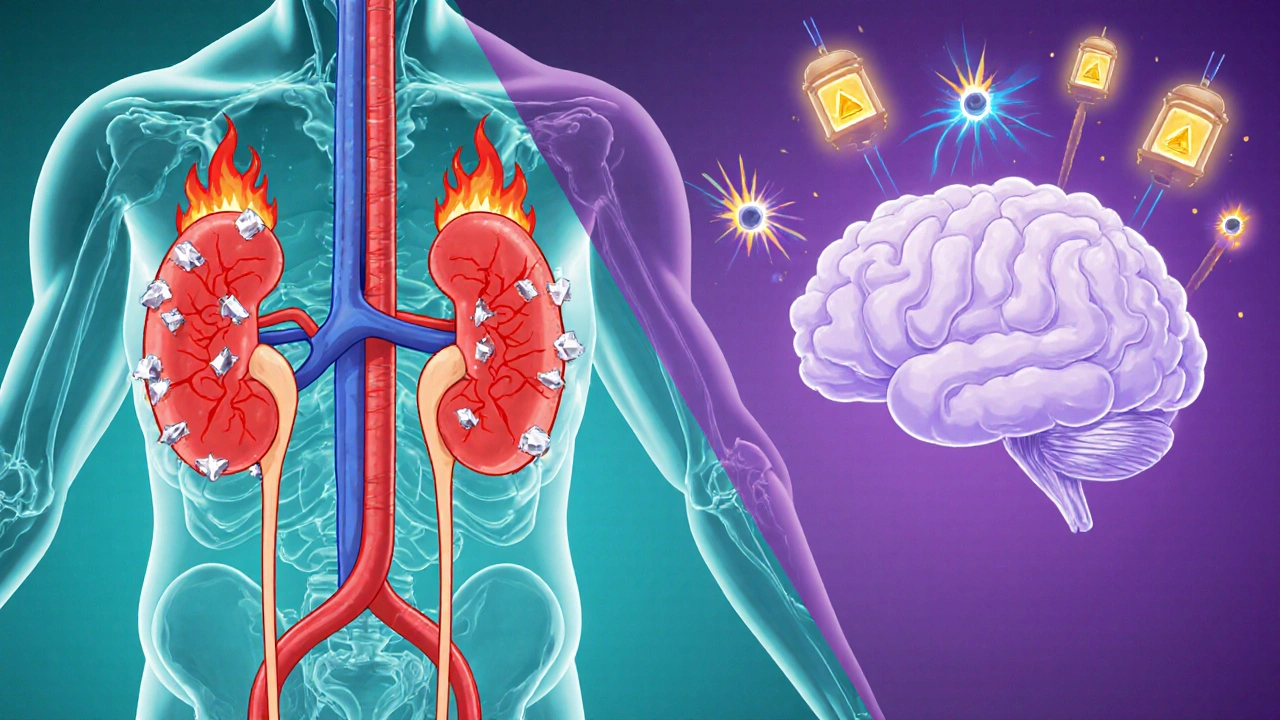
Neurologic complications that stack up
Fluoroquinolones have a notorious neuro‑toxic profile: seizures, confusion, psychosis, delirium, dyskinesias, and even Tourette‑like syndromes. The drugs inhibit GABA receptors and over‑activate NMDA receptors, making the brain more excitable. In patients with renal dysfunction, serum levels can jump 50‑100 % (FDA label), heightening the danger.
NSAIDs can cause headache (10‑15 % of users) and dizziness (5‑7 %). Rarely, they provoke aseptic meningitis, most often with ibuprofen or naproxen. When both medications accumulate, the risk of seizures and severe confusion spikes, especially in the elderly or those with pre‑existing neurological disease.
Case reports illustrate the nightmare: a 58‑year‑old man on ciprofloxacin 500 mg BID plus ibuprofen 400 mg TID for a UTI developed AKI (creatinine from 82 to 287 µmol/L) and peripheral neuropathy that lingered 18 months after stopping the drugs.
Real‑world stories and the impact on health systems
Patient‑led surveys paint a grim picture. The Fluoroquinolone Effects Research Foundation found 78 % of 1,245 respondents reported symptoms lasting beyond six months, with 32 % describing permanent disability. Online communities such as r/FQAntibioticDamage (14,500 + members) share daily accounts of “Fluoroquinolone‑Associated Disability” (FQAD): tendon pain, neuropathy, and cognitive fog.
From a macro view, adverse events cost the U.S. health system $1.8 billion a year (2020 Pharmacoepidemiology & Drug Safety). Renal complications alone accounted for 37 % of that expense, while neurologic damage contributed another 29 %.
Clinical guidance: how to avoid the double‑hit
Guidelines now advise keeping fluoroquinolones and NSAIDs apart whenever possible, especially for high‑risk groups:
- Patients > 60 years (renal clearance drops ~1 % per year after age 40)
- eGFR < 60 mL/min/1.73 m²
- History of seizures, peripheral neuropathy, or tendon disorders
When a fluoroquinolone is unavoidable, choose acetaminophen for pain rather than an NSAID. If an NSAID is needed, consider using a fluoroquinolone‑sparing antibiotic such as nitrofurantoin for uncomplicated UTIs or amoxicillin‑clavulanate for respiratory infections.
Monitoring is key: check baseline renal function, repeat serum creatinine 48‑72 hours after starting therapy, and watch for neurologic changes (confusion, tremor, new‑onset seizures). Early discontinuation can prevent permanent damage.
Risk‑mitigation checklist for prescribers
| Step | Action | Rationale |
|---|---|---|
| 1 | Screen for age > 60, eGFR < 60, or prior neurologic/kidney disease. | These factors amplify drug accumulation. |
| 2 | Ask about OTC NSAID use. | Patients often forget to mention ibuprofen or naproxen. |
| 3 | Choose an alternative antibiotic if pain control is needed. | Eliminates the additive nephro‑toxic effect. |
| 4 | Order baseline labs (creatinine, eGFR, electrolytes). | Detect early kidney injury. |
| 5 | Provide clear discharge instructions: stop both drugs if confusion, seizures, or sudden weight gain occur. | Patient‑driven early detection. |
Bottom line: stay alert, stay safe
If you or someone you care for needs a fluoroquinolone, double‑check whether an NSAID is also on the medication list. A quick conversation with the prescriber can save weeks or months of disability. Remember, the safest prescription is the one you don’t need.
What are the most common fluoroquinolones linked to kidney injury?
Ciprofloxacin and levofloxacin have the strongest evidence linking them to acute interstitial nephritis and crystal‑induced AKI, especially when taken with NSAIDs.
How much does the risk of AKI increase when fluoroquinolones and NSAIDs are combined?
Elderly patients on both drugs face up to a 3.5‑fold higher chance of hospitalization for AKI compared with using either drug alone.
Can the neurological side‑effects be reversed?
Stopping the fluoroquinolone early can halt progression, but some patients report lingering cognitive fog or peripheral neuropathy for months or years.
Are there safer pain relievers to use with fluoroquinolones?
Acetaminophen (paracetamol) is generally safe for most patients and does not affect renal prostaglandin pathways.
What monitoring should be done during therapy?
Check baseline serum creatinine and eGFR, repeat labs 48‑72 hours after starting the combo, and watch for new neurologic symptoms.






15 Comments
It's really unsettling how often these drug combos slip through the cracks, especially when patients are juggling other meds, and many of us just trust the prescription without a second thought. The evidence shows a clear uptick in kidney injury when fluoroquinolones meet NSAIDs, not to mention the neurologic fallout that can linger for months. I’ve seen friends struggle with persistent tingling and brain fog that just won’t go away, and those symptoms can make everyday tasks feel like climbing a mountain. What’s frustrating is that a simple medication change could have prevented all that. For anyone prescribed a fluoroquinolone, ask your doctor about alternative pain relievers; acetaminophen is usually a safer bet for the stomach and kidneys. If an NSAID is absolutely necessary, a short course at the lowest effective dose is key. Also keep an eye on your urine output and any sudden swelling. Getting a baseline creatinine before starting treatment gives you a reference point, and a follow‑up lab after a couple of days can catch trouble early. If you notice confusion, dizziness, or a headache that gets worse, call your provider right away. Staying proactive can mean the difference between a quick recovery and a long‑term disability. Don't assume side effects are rare; they happen more often than you think. Educate yourself on the signs of acute interstitial nephritis, like flank pain and fever. Remember that older adults have reduced renal clearance, making them especially vulnerable. A quick phone call to your pharmacist can also uncover hidden NSAID use from OTC purchases. Taking these steps not only protects your kidneys but also keeps your mind clear for the things you love.
I doubt the data is as scary as you make it sound. Doctors have been prescribing these combos for years without a pandemic of kidney failure.
The horror of mixing fluoroquinolones with NSAIDs reads like a medical nightmare, each dose a ticking time bomb waiting to explode. Patients report seizures that feel like electric shocks and kidneys that fail as if the filters were ripped out. The literature is flooded with case reports that sound more like horror stories than clinical studies. When the drugs accumulate, the brain goes into overdrive and the kidneys shut down, a double whammy you can't ignore. It's a catastrophe waiting to happen if we keep treating these meds like harmless over‑the‑counter fixes.
I see your point, the risks are real and we should definitely share them with patients before prescribing.
It’s heartbreaking to hear how many people suffer long‑term effects from something that could have been prevented. Let’s keep spreading awareness and encourage doctors to check for NSAID use before writing a fluoroquinolone. Together we can push for safer prescribing practices.
Indeed, one would assume the medical establishment is infallible and never errs in dosage decisions. Yet the data, whilst inconvenient, cannot be ignored. One might even suggest a thorough review of prescribing guidelines, if such a notion is not too radical. Sarcasm aside, vigilance remains paramount.
When I mentor junior pharmacists, I always stress the importance of looking beyond the obvious and questioning every drug interaction, especially those that silently undermine organ function. The fluoroquinolone‑NSAID pairing is a perfect illustration of how a seemingly benign combination can cascade into severe nephrotoxicity and neurotoxicity. Understanding the pharmacodynamics helps us predict who is at greatest risk, like the elderly or those with pre‑existing kidney disease. Moreover, integrating a simple checklist into the electronic health record can flag dangerous overlaps before the prescription is finalized. Encouraging patients to disclose any over‑the‑counter NSAID use also closes a critical gap in communication. By fostering a culture of double‑checking, we reduce the chance of iatrogenic harm. It’s not just about avoiding lawsuits; it’s about preserving quality of life for our community. Let’s champion this proactive stance in every clinical encounter.
While the official reports paint a reassuring picture, independent investigations have uncovered a pattern of suppressed adverse‑event data 😒. Some regulatory bodies appear reluctant to fully disclose the extent of renal damage linked to these molecules. This raises questions about the influence of pharmaceutical lobbying on public health policy. Consumers deserve transparent information, not curated narratives.
Current guidelines advise screening for renal insufficiency prior to initiating fluoroquinolone therapy. Measurement of serum creatinine and estimation of glomerular filtration rate provide essential baseline data. Subsequent monitoring at 48‑72 hours post‑prescription can identify acute kidney injury promptly.
Oh sure, because reading a dense guideline is exactly how most patients manage their meds. Yet a friendly reminder from a clinician can bridge that gap. Let’s keep the conversation light but informative.
We cant just ignore the moral duty we have to protect patiens from avoidable harm. It's our responsibilty to speak up when guidelines are flouted.
Great points everyone! I think we should all push for safer alternatives when possible :) Keep the discussion going.
Totally agree, safety first.
I appreciate the balanced perspective offered here. Maintaining open dialogue helps us all stay informed.
From a pharmacovigilance standpoint the drug‑drug interaction matrix indicates a synergistic nephrotoxic vector exacerbated by COX‑inhibition pathways 📊 clinicians should integrate real‑time eHR alerts to mitigate iatrogenic risk without overburdening workflow