Sensitive Skin: What Causes It and Which Medications Can Make It Worse
When your skin stings, burns, or turns red with little warning, you’re dealing with sensitive skin, a condition where the skin’s barrier is easily irritated by environmental, chemical, or pharmaceutical triggers. Also known as reactive skin, it’s not an official diagnosis but a common experience that affects millions—especially those on long-term medications or with autoimmune conditions. Unlike acne or eczema, sensitive skin doesn’t always show up on a doctor’s chart, but it can make daily life unbearable. You might use gentle cleansers, avoid fragrances, and still wake up with burning cheeks or itchy arms. The culprit? It’s often not what you’re putting on your skin—it’s what you’re taking inside.
Many medications silently worsen sensitive skin without people realizing it. NSAID sensitivity, a reaction where common painkillers like ibuprofen or aspirin trigger skin flare-ups or asthma attacks in some users, affects about 7% of asthma patients and can cause hives, swelling, or intense redness. If you’ve noticed your skin gets worse after taking Advil or Aleve, it’s not just coincidence. Similarly, methotrexate, a drug used for autoimmune diseases like psoriasis and rheumatoid arthritis, can cause dry, peeling, or blistering skin as a side effect. Even antidepressants like bupropion, while helping mood, can trigger rashes or increased skin reactivity in some people. These aren’t rare oddities—they’re documented reactions that show up in patient reports and FDA labels.
What makes sensitive skin even trickier is that it often overlaps with other conditions. Someone with dermatomyositis might have a rash that looks like sunburn but is actually immune-driven. A person on long-term steroids might develop thin, easily bruised skin that tears with minor friction. And if you’re breastfeeding or managing kidney function as a senior, your body processes drugs differently—making skin reactions more likely. The same drug that helps one person might irritate another’s skin because of genetics, age, or other meds they’re taking.
You don’t have to live with skin that feels like it’s on fire. The key is connecting the dots between what you’re taking and how your skin reacts. Tracking when flare-ups happen—after starting a new pill, after a dose change, or after switching generics—can reveal patterns your doctor might miss. You have the right to ask: Could this drug be causing my skin to react? And if so, is there a safer alternative?
Below, you’ll find real-world guides from people who’ve been there—how to spot drug-induced skin reactions, which painkillers are safest for reactive skin, how to tell if your rash is from medication or something else, and what to say when your pharmacy tries to switch your brand to a generic without warning. This isn’t about avoiding treatment—it’s about getting the treatment you need without paying for it in itchy, burning skin.
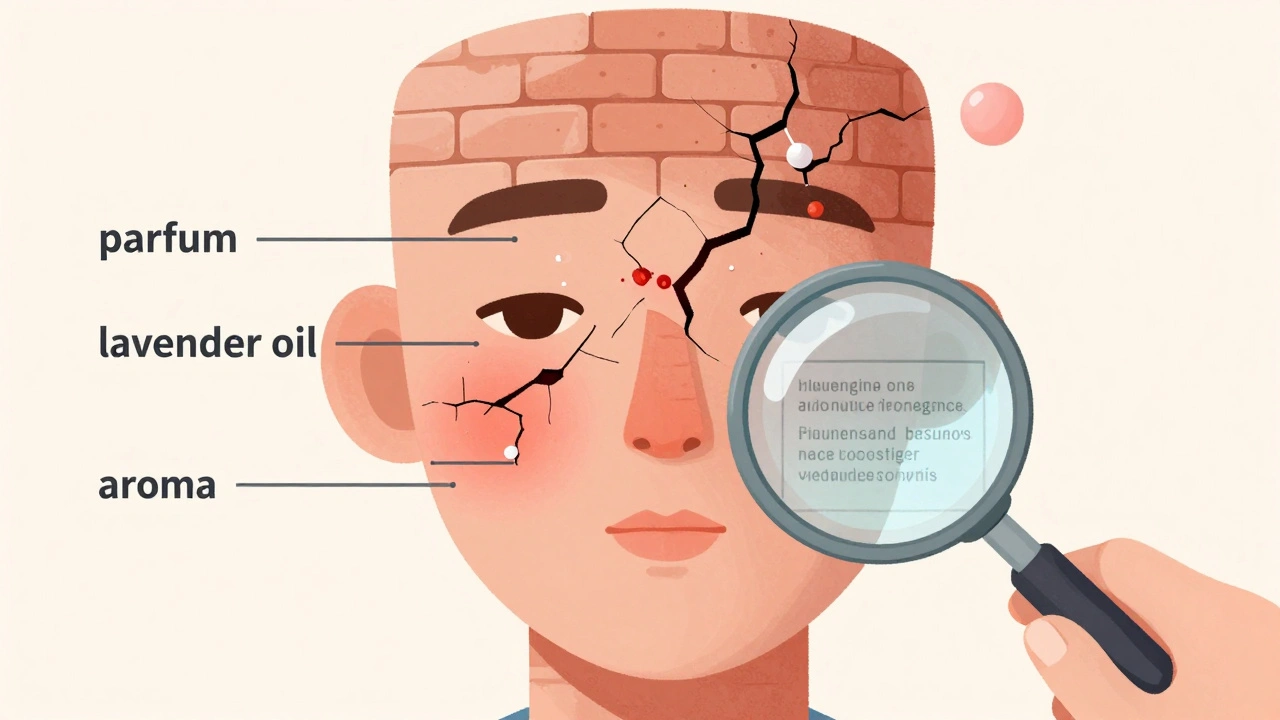
Fragrance-Free Skin Care for Sensitive Skin: Simple Routines and How to Test Products
Fragrance-free skincare routines help sensitive skin by removing common irritants. Learn how to test products, choose safe formulas, and build a simple routine that reduces redness and irritation.
read more




