NSAID Kidney Risk: What You Need to Know Before Taking Pain Relievers
When you reach for ibuprofen or naproxen for a headache or sore back, you’re using a type of drug called a NSAID, nonsteroidal anti-inflammatory drugs that reduce pain, fever, and inflammation. Also known as nonsteroidal anti-inflammatories, these drugs are among the most common medications people take daily—but they can quietly damage your kidneys, especially if you’re older, dehydrated, or have existing health issues. Unlike liver damage, which often shows up with obvious symptoms like yellow skin or nausea, kidney harm from NSAIDs happens slowly. By the time you feel it, the damage might already be done.
The real danger isn’t just taking one pill now and then. It’s daily use over months or years. People with high blood pressure, diabetes, heart failure, or chronic kidney disease are at higher risk. Even healthy adults aren’t safe if they take NSAIDs regularly without knowing the toll. Studies show that long-term NSAID users are up to 30% more likely to develop kidney problems than non-users. And here’s the twist: your doctor might not warn you. Most patients assume painkillers are harmless because they’re sold over the counter.
That’s why it’s critical to understand how kidney function, how well your kidneys filter waste and balance fluids connects to these drugs. NSAIDs reduce blood flow to the kidneys by blocking protective chemicals called prostaglandins. In healthy people, this isn’t a big deal. But if you’re already low on fluid—because you didn’t drink enough water, are sweating a lot, or are on a diuretic—your kidneys can’t compensate. That’s when trouble starts. Signs like swelling in your ankles, fatigue, or changes in urination can be early red flags. Many people ignore them, thinking it’s just aging or stress.
And it’s not just about the drug itself. Your other medications matter too. If you’re taking blood pressure pills like ACE inhibitors or diuretics, combining them with NSAIDs raises your risk even more. This isn’t theoretical—it’s why hospitals track NSAID use in seniors with heart or kidney conditions. The eGFR, a standard test that estimates how well your kidneys are filtering blood is the best way to catch early damage. But most people never get it checked unless they’re already sick.
You don’t have to avoid NSAIDs completely. But you need to use them smarter. Take the lowest dose for the shortest time. Stay hydrated. Avoid them if you’re dehydrated or sick with vomiting or diarrhea. Talk to your doctor before using them daily—even if you bought them without a prescription. There are safer alternatives for chronic pain, like acetaminophen (though it has its own risks), physical therapy, or even targeted supplements.
In the posts below, you’ll find real-world advice from people who’ve dealt with NSAID-related kidney issues, guides on how to monitor your kidney health, and clear comparisons between pain relief options that won’t put your kidneys at risk. These aren’t theory pieces—they’re practical, tested tips from patients and clinicians who’ve seen the damage firsthand. Whether you’re taking NSAIDs now or just thinking about it, this collection gives you the tools to protect yourself before it’s too late.
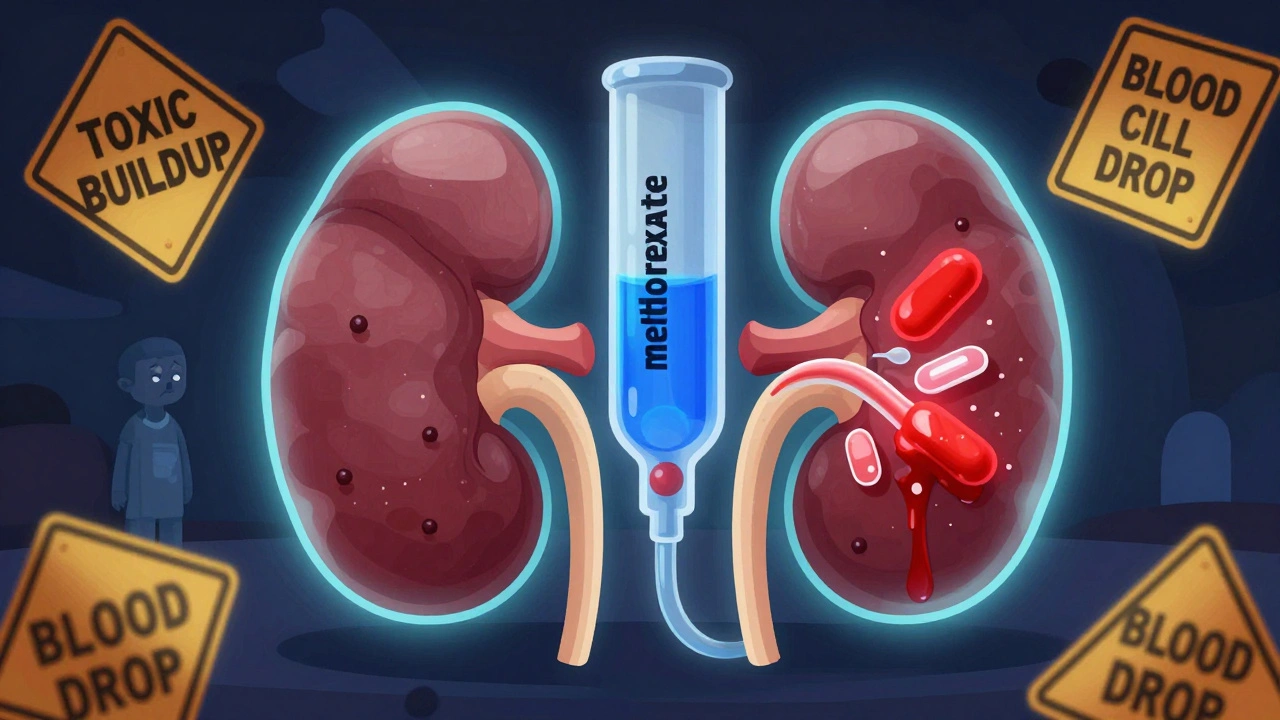
Methotrexate and NSAIDs: What You Need to Know About Renal Toxicity and Drug Levels
Methotrexate and NSAIDs can cause dangerous kidney toxicity and elevated drug levels. Learn who's at risk, which painkillers are safest, and how to prevent life-threatening side effects.
read more




