Dermatomyositis and polymyositis are rare autoimmune diseases that cause chronic inflammation in skeletal muscles, leading to progressive weakness and, in the case of dermatomyositis, distinct skin rashes. These conditions don’t show up overnight. They creep in slowly-first, you can’t climb stairs like you used to. Then, getting up from a chair feels like lifting a weight. For many, the first sign isn’t pain, but fatigue and frustration. By the time a diagnosis comes, months or even years have passed. And that delay is common. About 30% of people are misdiagnosed early on, often told it’s fibromyalgia, thyroid trouble, or just aging.
What Sets Dermatomyositis Apart from Polymyositis?
Both conditions attack the same muscles-proximal ones, meaning those closest to your torso: hips, thighs, shoulders, neck. But dermatomyositis adds a visible layer. A purple or red rash shows up on eyelids, knuckles, elbows, knees, or the upper chest. This is called a heliotrope rash. It’s not itchy or scaly like eczema. It’s flat, distinct, and often appears before muscle weakness. In children, it can be the only sign.
Polymyositis? No rash. Just muscle decline. That’s why it’s harder to spot. People often ignore it until they drop things, struggle to lift their arms, or need help standing after sitting. Both conditions are more common in women-two to three times more than men. Dermatomyositis hits in two waves: kids aged 5 to 15, and adults between 40 and 60. Polymyositis almost never affects children. It starts in adulthood.
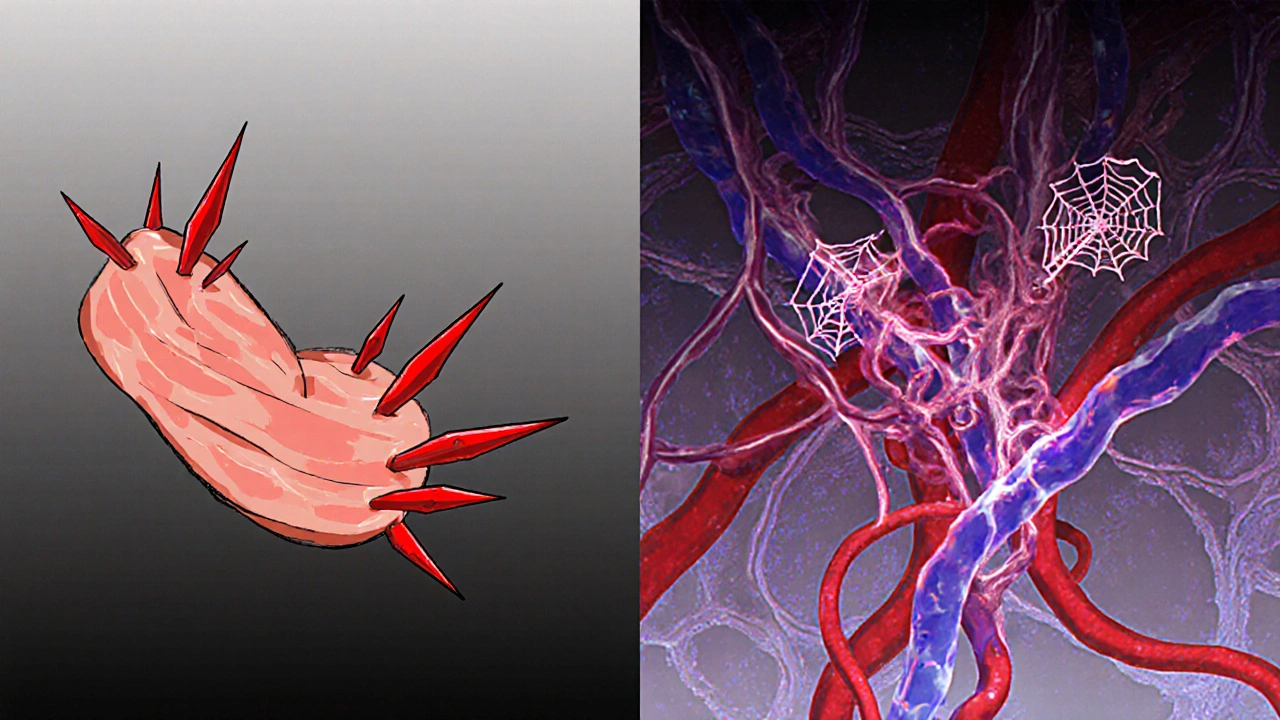
The difference isn’t just skin deep. Under the microscope, the immune system behaves differently. In dermatomyositis, B cells and antibodies attack blood vessels around muscle fibers. In polymyositis, T cells invade and destroy muscle cells directly. That’s why treatments can vary.
How Is It Diagnosed?
There’s no single blood test that says "yes, you have dermatomyositis." Diagnosis is a puzzle. First, doctors check for elevated creatine phosphokinase (CPK). Normal levels are 10-120 U/L. In active disease, they can jump to 8,000 or higher. Other markers like ESR and CRP show inflammation. ANA (antinuclear antibody) is often positive, but that’s not specific-it shows up in lupus and other autoimmune diseases too.
Next comes electromyography (EMG). This test measures electrical activity in muscles. In myositis, it picks up short, low-amplitude signals and spontaneous firing-signs of damaged, irritated muscle tissue.
But the real gold standard is a muscle biopsy. A small piece of muscle, usually from the thigh or shoulder, is taken under local anesthesia. In polymyositis, you see T cells clustering around healthy muscle fibers. In dermatomyositis, you see damaged muscle fibers at the edges of muscle bundles (perifascicular atrophy) and inflammation around small blood vessels.
And here’s something critical: about 1 in 5 adults with dermatomyositis have an underlying cancer. That’s why doctors don’t just treat the muscle-they screen for tumors. Lung, ovarian, breast, and colon cancers are the most common. A full-body scan, mammogram, pelvic ultrasound, or colonoscopy might be part of the initial workup.
What Does Treatment Look Like Today?
There’s no cure. But there’s control. And early treatment makes all the difference. Studies show that if you start treatment within six months of symptoms, 80% of patients reach low disease activity or remission. Delayed treatment? That’s when muscle damage becomes permanent.
The first-line drug is always corticosteroids-usually prednisone. Doctors start with 1 mg per kilogram of body weight daily. For a 70 kg adult, that’s about 70 mg a day. That’s high. And it’s not meant to last. After 4 to 8 weeks, the dose is slowly lowered. The goal isn’t to eliminate the drug completely, but to find the lowest dose that keeps inflammation under control.
But steroids come with a price. Half of long-term users develop osteoporosis. One in three get diabetes. Two in five develop cataracts. That’s why calcium, vitamin D, and bone-density scans are part of the plan from day one.
That’s where second-line drugs come in. Methotrexate is the most common. It’s taken weekly, orally or by injection. Azathioprine and mycophenolate mofetil are alternatives. These drugs take weeks to months to work, but they let doctors reduce steroid doses faster.
For stubborn cases, especially in dermatomyositis, IVIG (intravenous immunoglobulin) is used. It’s a concentrated mix of antibodies from healthy donors. It doesn’t cure, but it can quiet the immune system. One patient in Adelaide, after failing three steroid trials, started IVIG every four weeks. Within three months, her rash faded and she could lift her arms again.
Rituximab, a drug used in lymphoma and rheumatoid arthritis, is showing promise too. In trials, 60-70% of refractory dermatomyositis patients improved. It’s off-label, but many rheumatologists use it when other options fail.
And now, new players are entering the game. JAK inhibitors like tofacitinib, originally for arthritis, are being tested in dermatomyositis. In a 2023 trial, patients saw 65% improvement in skin rashes and over 50% gain in muscle strength. Abatacept, which blocks T-cell activation, is being studied in polymyositis with early results showing 40% of patients reaching minimal disease activity.
Physical Therapy Isn’t Optional-It’s Essential
Medication alone won’t restore strength. Muscle that’s not used atrophies. And once it’s gone, it’s hard to get back. That’s why physical therapy starts within two weeks of diagnosis.
It’s not about heavy weights or intense cardio. It’s gentle, controlled movement: seated leg lifts, wall push-ups, resistance bands for shoulders. The goal is to prevent stiffness and maintain function without triggering more inflammation. Studies show structured programs improve functional capacity by 35-45% in six months.
Many patients report that the hardest part isn’t the meds-it’s the fatigue. Over two-thirds of people in a 2022 survey said fatigue limited daily tasks. That’s why pacing matters. Rest when you need to. Don’t push through pain. A physical therapist can help you find the balance.
Living With It: The Hidden Struggles
Most people think of muscle weakness. But there’s more. Swallowing problems-dysphagia-affect 15-30% of patients. Food gets stuck. Choking risks rise. Speech pathologists are often part of the care team, teaching safe swallowing techniques.
Interstitial lung disease shows up in 30-40% of dermatomyositis cases. It’s silent at first. No cough. No fever. But over time, it can cause shortness of breath. Regular lung function tests are standard.
And then there’s the emotional toll. A 2023 survey of over 1,200 patients found that 41% had moderate to severe side effects from steroids-weight gain, insomnia, mood swings. One Reddit user wrote: "I gained 40 pounds in six months. I stopped looking in mirrors. My husband said I looked like a different person. That hurt more than the muscle pain."
Support groups help. The Myositis Support and Understanding Association has forums where people share stories, tips, and validation. Many say finding others who "get it" was the turning point in their journey.

What’s Changing in 2025?
The diagnostic game is changing. In June 2023, the European League Against Rheumatism updated its guidelines to include myositis-specific antibodies (MSAs) as key diagnostic markers. These are autoantibodies that target specific proteins inside muscle cells. Anti-Mi-2? Strongly linked to classic dermatomyositis. Anti-Jo-1? Often found in polymyositis with lung involvement. Testing for these can cut diagnostic delays by 30-40%.
Drug development is slow, but moving. Only three drugs are FDA-approved for dermatomyositis-none for polymyositis. Most treatments are used off-label. Insurance still fights back. A 2022 study found patients wait an average of 17 days for prior authorization on second-line drugs.
And there’s a shortage of specialists. In the U.S., there’s one rheumatologist for every 10,000 people with autoimmune conditions. In Australia, access is better in cities like Adelaide, but rural patients still face long waits.
But the prognosis is better than ever. In the 1970s, only half of patients survived 10 years. Today, over 80% do. With early diagnosis, smart medication, physical therapy, and support, most people can live full, active lives.
What Should You Do If You Suspect You Have It?
If you’ve had unexplained muscle weakness for more than a few weeks, especially with a rash, fatigue, or trouble swallowing:
- See your GP. Ask for a CPK blood test.
- If CPK is high, request a referral to a rheumatologist-not a neurologist or physiotherapist. This is an autoimmune disease.
- Insist on a muscle biopsy if diagnosis is unclear.
- Ask about cancer screening if you’re an adult with dermatomyositis.
- Start physical therapy early. Don’t wait for meds to kick in.
- Join a support group. You’re not alone.
It’s not a death sentence. It’s a chronic condition. And like diabetes or hypertension, it’s manageable-with the right team, the right timing, and the right mindset.
Can dermatomyositis and polymyositis be cured?
No, there is no cure for either condition. But with early and aggressive treatment, most patients can achieve remission or low disease activity. Muscle strength can improve significantly, and many people return to normal daily activities. The goal is long-term control, not a cure.
Is dermatomyositis contagious?
No, dermatomyositis is not contagious. It’s an autoimmune disease, meaning your own immune system mistakenly attacks your muscles and skin. You can’t catch it from someone else, and you can’t give it to others.
Can children get polymyositis?
Polymyositis almost never occurs in children. It primarily affects adults between the ages of 30 and 60. Children can get dermatomyositis, which has a peak incidence between ages 5 and 15. The pediatric form is called juvenile dermatomyositis and is treated similarly to the adult version.
Why do I need a muscle biopsy if my blood tests are high?
High CPK levels mean muscle damage is happening, but not why. Many conditions-viral infections, overexertion, even certain medications-can raise CPK. A biopsy confirms the inflammation is autoimmune in nature and distinguishes between dermatomyositis and polymyositis. It’s the only way to see the immune cells attacking the muscle tissue under the microscope.
How long does it take to see improvement after starting treatment?
Steroids usually start working within 2-4 weeks. Muscle strength and rash improvement are often noticeable by week 6. But second-line drugs like methotrexate can take 3-6 months to reach full effect. Blood tests like CPK should drop by at least 50% within 4-8 weeks if treatment is working.
Can I exercise with dermatomyositis or polymyositis?
Yes, but carefully. Low-resistance, controlled exercise is critical to prevent muscle loss and maintain function. Avoid high-intensity workouts or heavy lifting during active flare-ups. A physical therapist experienced in autoimmune myopathies can design a safe program tailored to your strength level and disease activity.
Are there any new drugs on the horizon?
Yes. JAK inhibitors like tofacitinib are showing strong results in dermatomyositis, especially for skin and muscle symptoms. Abatacept, which blocks T-cell signaling, is being tested in polymyositis. Clinical trials are also exploring newer biologics and targeted therapies. While none are FDA-approved yet for these conditions, many rheumatologists are using them off-label in resistant cases.
What’s the long-term outlook for someone with these conditions?
The outlook has improved dramatically. Ten-year survival rates are now over 80% for dermatomyositis and 85% for polymyositis-up from 50-60% in the 1970s. With early treatment, most patients avoid permanent disability. The biggest challenges are managing steroid side effects and preventing lung complications. Regular follow-ups and adherence to therapy are key.


13 Comments