Why Lung Cancer Screening Matters More Than Ever
Most people don’t realize that lung cancer kills more people each year than breast, colon, and prostate cancer combined. And yet, if caught early, survival rates jump from just 6% to nearly 60%. The problem? Only about 1 in 5 cases are found early. That’s mostly because symptoms don’t show up until the cancer is advanced. For smokers and former smokers, the key to changing those odds is simple: annual low-dose CT scans. But even with clear guidelines, most eligible people aren’t getting screened.
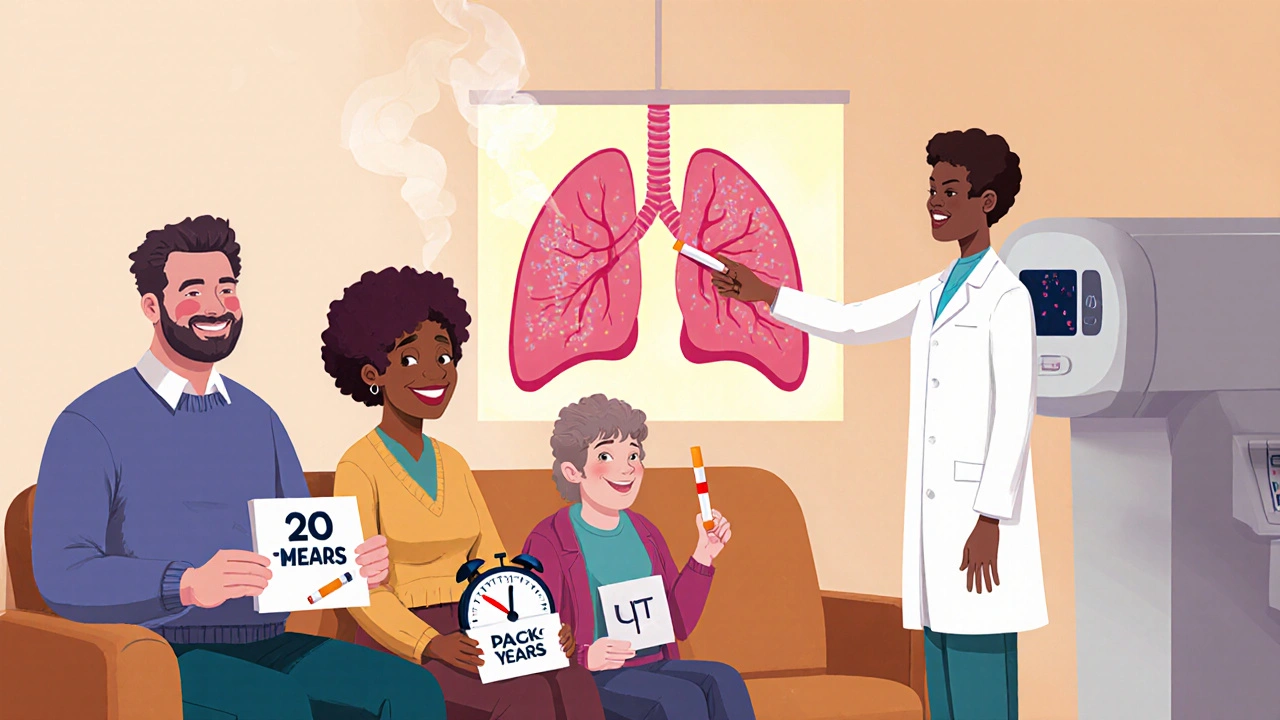
Who Should Be Screened? The Updated Rules
In 2023, the American Cancer Society updated its lung cancer screening guidelines - and they’re now the most inclusive in the U.S. You qualify if you’re between 50 and 80 years old, have smoked at least 20 pack-years, and either still smoke or quit within the last 15 years. A pack-year means smoking one pack a day for a year. So if you smoked two packs a day for 10 years, you hit that threshold. Or half a pack a day for 40 years. It’s not about how long you smoked - it’s about total exposure.
What changed from older rules? The big one is the removal of the 15-year quit cutoff. Before, if you quit smoking 16 years ago, you were no longer eligible. But research shows former smokers remain at high risk for decades. A 2022 JAMA Oncology study found people who quit 15 to 30 years ago still had 2.5 times the risk of lung cancer compared to people who never smoked. That’s why the ACS now recommends screening for all eligible former smokers, no matter how long ago they quit.
How Screening Works: The Low-Dose CT Scan
The only proven method for early lung cancer detection is a low-dose CT scan, or LDCT. It’s quick - takes less than 10 seconds. You lie on a table, hold your breath, and that’s it. The machine uses 70-80% less radiation than a regular CT scan. No needles, no fasting, no prep. It’s designed to find tiny nodules in the lungs before they grow into tumors.
But here’s the catch: most positive results aren’t cancer. The National Lung Screening Trial showed that 96.4% of positive scans turned out to be false alarms. That means a lot of follow-up tests, biopsies, and anxiety. That’s why screening should only happen at accredited centers with protocols for managing results. The American College of Radiology requires specific scan settings: 120 kVp, 30-50 mAs, and slice thickness between 1.25 and 2.5 mm. Not every hospital or imaging center meets these standards.
Why So Few People Are Getting Screened
Despite the guidelines, only about 5.7% of eligible Americans - roughly 2.6 million out of 45.5 million - got screened in 2021. Why? Three big reasons.
- Doctors don’t bring it up. A 2022 AMA survey found 42% of primary care doctors didn’t even know the updated USPSTF guidelines. If your doctor doesn’t mention it, you won’t know you’re eligible.
- Access is limited. There are only about 2,800 ACR-accredited screening centers in the entire U.S. Rural areas have 67% fewer facilities than cities. If you live outside a major metro, getting a scan can mean driving hours.
- Insurance confusion. Medicare covers screening for people aged 50-77 with a 20-pack-year history. But some private insurers still follow the old 55-80 age range and 30-pack-year rule. You might be eligible, but your plan won’t pay.
The Role of AI and Better Tools
Artificial intelligence is starting to make screening smarter. In January 2023, the FDA approved the first AI tool for lung nodule detection - LungQ by Riverain Technologies. It helps radiologists spot subtle changes faster and reduces false positives by 15-20%. That means fewer unnecessary biopsies and less stress for patients.
Other tools are in the works. The National Cancer Institute is running the PACIFIC trial, launching in mid-2024, to test whether adding genetic risk markers and environmental exposures can better identify who needs screening. Right now, smoking history is the only filter. But what if we could also measure your DNA risk? Or your exposure to radon or air pollution? That’s the next step.
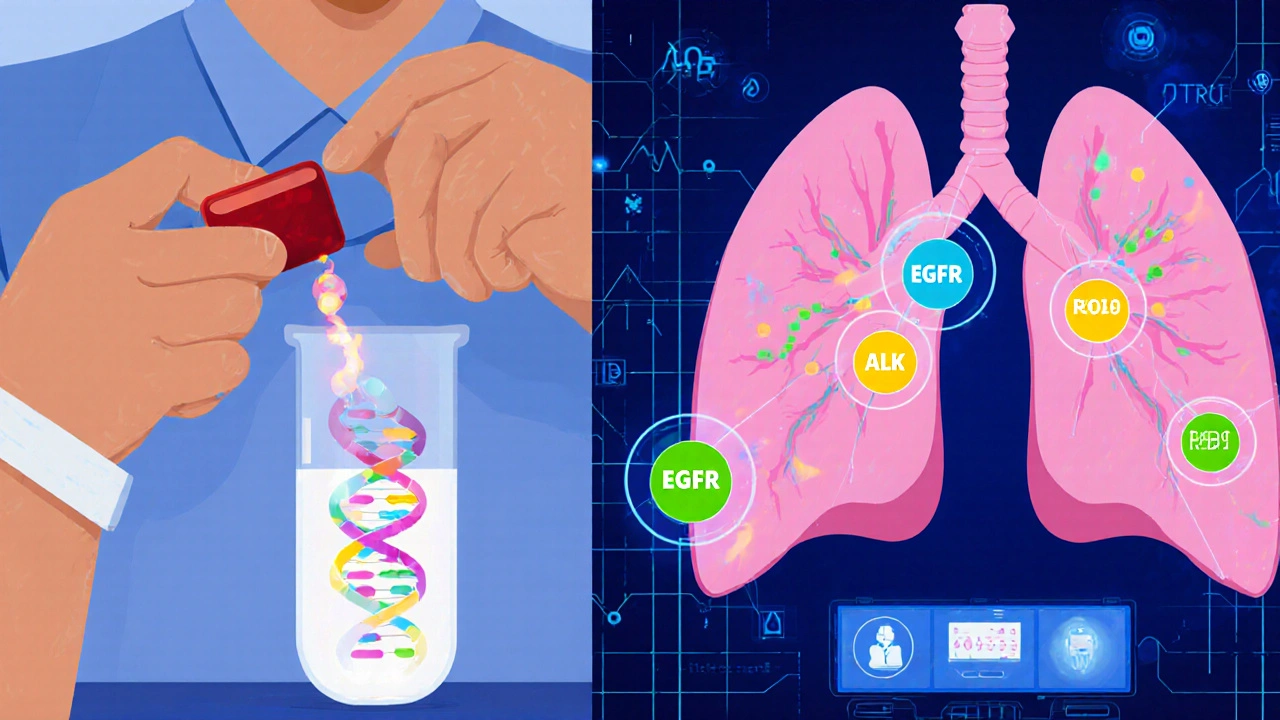
Targeted Therapy: Turning Early Detection Into Long-Term Survival
Screening finds cancer early. But what happens next? That’s where targeted therapy has changed everything. If your tumor has a specific genetic mutation - like EGFR, ALK, or ROS1 - you can take a pill instead of chemotherapy. These drugs attack only cancer cells, not healthy ones. Side effects are much milder, and survival rates are dramatically better.
The ADAURA trial, published in the New England Journal of Medicine in 2021, showed that for patients with early-stage EGFR-mutated lung cancer, taking osimertinib after surgery cut the risk of recurrence or death by 83%. That’s not just a small improvement - it’s life-changing. The FDA approved osimertinib for this use in December 2020, and now it’s standard care for eligible patients.
Here’s the exciting part: by 2025, the International Association for the Study of Lung Cancer predicts that 70% of early-stage lung cancers found through screening will have these actionable mutations. But only 30% of late-stage cancers do. That means the earlier you catch it, the more likely you are to benefit from a targeted pill. Screening isn’t just about finding cancer - it’s about finding the right treatment before it spreads.
What’s Next: Liquid Biopsies and Personalized Screening
The future of lung cancer care is moving beyond imaging. Researchers are testing liquid biopsies - blood tests that detect tumor DNA floating in the bloodstream. These tests could spot cancer months before a CT scan shows anything. Trials like NCT04541082 and NCT04924022 are already underway, testing whether combining liquid biopsy with LDCT can catch cancer even earlier.
Imagine a future where your screening includes:
- A risk calculator that factors in smoking, genetics, and environment
- A blood test to check for cancer DNA
- An annual LDCT scan
- If something shows up, immediate genetic testing to match you with the right targeted therapy
By 2030, the American Society of Clinical Oncology expects this kind of integrated approach to push five-year survival rates from today’s 23% to over 40%. That’s not science fiction - it’s the roadmap.

What You Can Do Right Now
If you’re a current or former smoker aged 50-80 with a 20-pack-year history, talk to your doctor. Don’t wait for them to bring it up. Ask: "Am I eligible for lung cancer screening?" If they say no, ask why. Check your insurance plan. If you’re in a rural area, look up ACR-accredited centers using the American College of Radiology’s online directory.
If you’re still smoking, screening isn’t a substitute for quitting. But it’s a powerful reason to stop. The American Thoracic Society says 70% of screened smokers want to quit - yet only 30% get help. Ask for a referral to a cessation program. Many screening centers now offer counseling and nicotine replacement as part of the service.
Key Takeaways
- Annual low-dose CT scans can cut your risk of dying from lung cancer by 20%.
- You qualify if you’re 50-80, smoked 20+ pack-years, and still smoke or quit within the last 15 years (ACS guidelines).
- False positives are common - always go to an accredited center with follow-up protocols.
- Targeted therapies like osimertinib can prevent recurrence in early-stage cases with specific mutations.
- AI tools are reducing unnecessary scans, and liquid biopsies may soon detect cancer before it’s visible.
Frequently Asked Questions
Do I need a prescription for a lung cancer screening CT scan?
Yes. You need a referral from your doctor. Screening isn’t something you can just walk in for. Your doctor will review your smoking history, assess your risk, and order the scan if you qualify. Some clinics require a shared decision-making visit - a 15-minute discussion about the benefits and risks - before scheduling.
Is lung cancer screening covered by insurance?
Medicare covers annual LDCT scans for beneficiaries aged 50-77 with a 20-pack-year history who currently smoke or quit within the past 15 years. Most private insurers follow the USPSTF 2021 guidelines and cover screening too. But some still use older rules (like requiring 30 pack-years). Call your insurer and ask: "Do you cover lung cancer screening under USPSTF 2021 guidelines?" If they say no, ask for a written explanation.
What if I quit smoking more than 15 years ago?
Under the USPSTF guidelines, you’re no longer eligible. But under the American Cancer Society’s 2023 guidelines, you still qualify - as long as you’re 50-80 and have a 20-pack-year history. Many experts now believe the 15-year cutoff is outdated. If you’re in good health and your doctor agrees, you may still benefit from screening even if your insurer doesn’t cover it.
Can I get screened if I’ve never smoked?
Current guidelines focus on smokers and former smokers because they make up 80-90% of cases. But about 10-20% of lung cancers occur in people who never smoked. For those with strong risk factors - like radon exposure, family history, or asbestos exposure - some centers offer screening on a case-by-case basis. Talk to your doctor if you have concerns.
What happens if the scan finds a nodule?
Most nodules are benign. If one is found, you’ll get a follow-up scan in 3-6 months to see if it grows. If it does, you may need a biopsy or PET scan. Only about 3-4% of screened people end up with cancer. The key is not panicking - follow the recommended timeline. Programs with patient navigators help guide you through this process and reduce anxiety.






12 Comments