
Opioid Nausea Prevention Calculator
How This Works
Based on your opioid type and dose, this calculator shows the optimal time to take your antiemetic to prevent nausea. Studies show timing antiemetics 30-60 minutes before opioid doses improves symptom control by up to 40%.
When you start taking opioids for pain, nausea isn’t just an inconvenience-it can stop you from taking the medicine you need. About 30-40% of people new to opioids feel sick to their stomach within the first day or two. For many, it’s so bad they skip doses or quit entirely. But this isn’t something you have to live with. With the right strategy, you can reduce or even eliminate opioid-induced nausea without giving up pain control.
Why Opioids Make You Nauseous
Opioids don’t just block pain signals-they also hit receptors in your brainstem called the chemoreceptor trigger zone. This area doesn’t care if you’re in pain or not. When opioids bind to it, your brain thinks something toxic is in your system and triggers vomiting. It’s a reflex, not a sign of overdose or bad medicine. This reaction usually hits hardest in the first 24 to 48 hours after starting or increasing your dose. After three to seven days, most people’s bodies adapt. But waiting it out isn’t always practical-especially if you’re already in pain and can’t eat or sleep.Which Antiemetics Work Best
Not all anti-nausea drugs are created equal for opioid-induced nausea. The most effective ones target the brain’s vomiting center directly.- Haloperidol (0.5-2 mg daily): A low-dose antipsychotic that blocks dopamine. It’s cheap-around $0.05 per tablet-and works well for most people. But it can cause stiffness or tremors in older adults, especially over 65.
- Prochlorperazine (5-10 mg every 6-8 hours): A phenothiazine that’s often preferred for its balance of effectiveness and safety. It’s a solid first choice for many doctors.
- Metoclopramide (5-10 mg every 6-8 hours): This one speeds up your stomach emptying, which helps if nausea comes with bloating or delayed digestion. It’s the only prokinetic available in the U.S., but it carries a risk of muscle spasms at higher doses.
- Ondansetron (4-8 mg every 8 hours): Often used for chemo nausea, it’s less reliable for opioid-induced nausea. It works better for sudden, sharp episodes than for constant nausea.
Cost matters. Generic haloperidol costs pennies. Brand-name ondansetron can run over $3 per tablet. If you’re paying out of pocket, choose wisely.
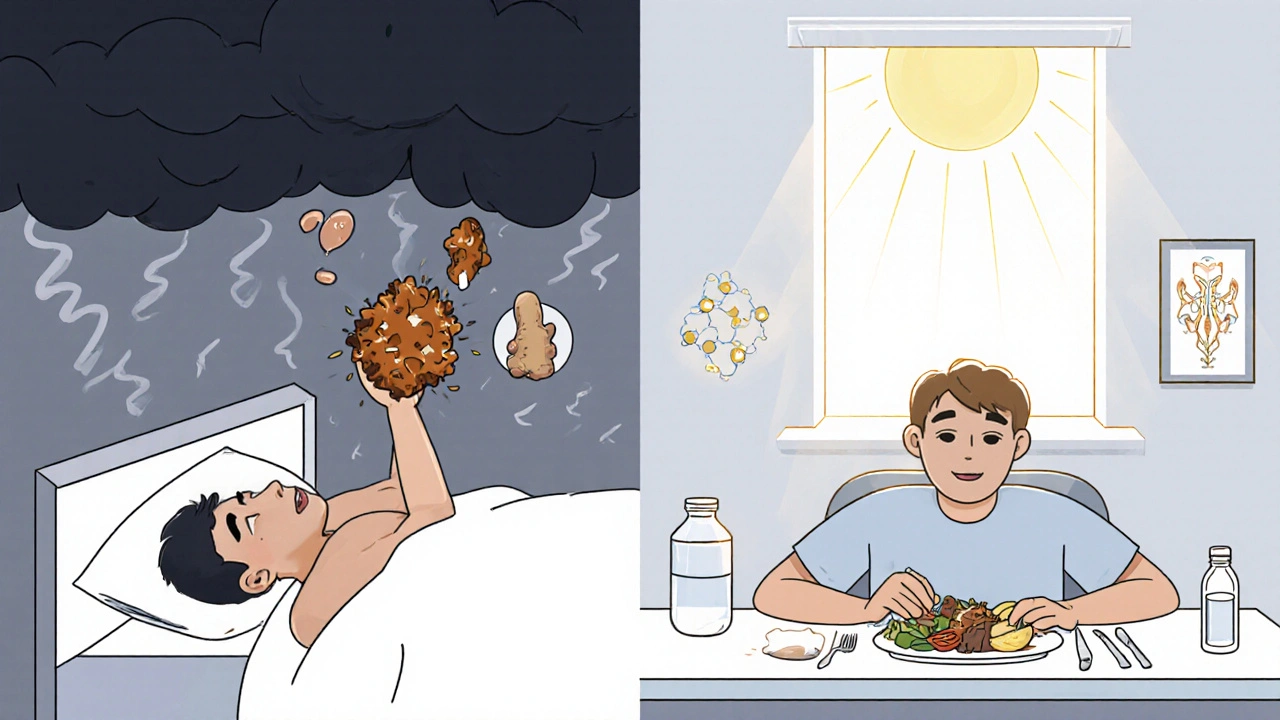
Timing Matters More Than You Think
Taking your antiemetic at the same time as your opioid isn’t enough. You need to get the drug into your system before the opioid peaks.Opioids like morphine or oxycodone reach their highest blood levels about 60 to 90 minutes after you swallow them. That’s when nausea hits hardest. So if you take your opioid at 8 a.m., take your antiemetic at 7 a.m. That way, the anti-nausea medicine is already working when the opioid kicks in.
This isn’t just theory. Studies show that timing antiemetics 30-60 minutes before opioid doses improves symptom control by up to 40%. It’s a simple trick-but most patients aren’t told to do it.
Diet Adjustments That Help
What you eat-and when-can make a big difference.- Eat small, bland meals. Avoid greasy, spicy, or sweet foods. Stick to crackers, toast, rice, or broth. These are easier to keep down.
- Don’t eat right before or after your opioid. Wait at least an hour after taking your pain medicine before eating. Eating too soon can trigger nausea when your stomach is already sensitive.
- Stay upright after meals. Lying down slows digestion and makes nausea worse. Sit up for at least 30 minutes after eating.
- Try ginger. Ginger tea or capsules (250-500 mg) have been shown in small studies to reduce nausea in opioid users. It’s not a replacement for medication, but it can help as a side support.
- Hydrate slowly. Sip water, clear broth, or electrolyte drinks. Chugging fluids can make you feel fuller and more nauseous.
One overlooked point: constipation from opioids can worsen nausea. A full, sluggish gut sends signals to your brain that mimic poisoning. If you’re constipated, treating that with stool softeners or laxatives often reduces nausea too.
When to Switch Opioids
If nausea sticks around after a week-even with antiemetics and diet changes-it might be time to switch opioids. Not all opioids cause nausea the same way.- Morphine is the most likely to cause nausea.
- Oxycodone is slightly better tolerated.
- Hydromorphone (Dilaudid) may reduce nausea in 40-50% of patients who switch from morphine.
- Methadone is often the best choice for long-term use, but switching requires careful dosing by a specialist.
Switching isn’t a quick fix. It takes 3-5 days for the new drug to build up in your system. You’ll need to overlap doses carefully to avoid withdrawal or overdose. Only do this under medical supervision.
Why Prophylactic Antiemetics Often Fail
You might think: “Why not just give everyone an antiemetic from day one?” That’s what many doctors do. But studies show it doesn’t prevent nausea-it just treats it after it starts.A 2019 review of 619 patients found that giving antiemetics before opioids started didn’t reduce nausea rates. In fact, it was statistically worse than waiting to treat symptoms as they appeared (p=0.037). Why? Because the body’s response to opioids varies. Some people need help, others don’t. Giving drugs to everyone means exposing people to side effects for no reason.
The smarter move? Start with low-dose opioids and only add antiemetics if nausea appears. This cuts down on unnecessary medication and keeps things simpler.
The Low-Dose Start Strategy
One of the most effective ways to avoid nausea is to start low and go slow.Instead of starting with 10 mg of morphine every 4 hours, begin with 2.5-5 mg. Increase by no more than 25-50% every 24-48 hours. This approach cuts nausea by 35-40% compared to standard dosing.
It takes longer to reach full pain control-often 7 to 10 days-but most patients find it’s worth it. You’re not just avoiding nausea. You’re giving your body time to adjust without being overwhelmed.

When to Call Your Doctor
Nausea is common. But if you experience any of these, reach out immediately:- Vomiting more than twice a day for more than 2 days
- Unable to keep down fluids for 12+ hours
- Dizziness, confusion, or extreme drowsiness along with nausea
- Muscle stiffness, tremors, or uncontrolled movements (signs of dopamine blocker side effects)
- Nausea that gets worse after a week, even with treatment
These aren’t normal. They could mean you need a different antiemetic, a different opioid, or a dose adjustment.
What Doesn’t Work
There are a lot of myths out there.- Antihistamines like Benadryl help with motion sickness or allergies, but they rarely help with opioid nausea.
- Corticosteroids like dexamethasone can help in some cases, but their mechanism isn’t clear. They’re not a first-line option.
- Waiting it out without any support leads to 30-35% of cancer patients quitting opioids entirely. That’s not bravery-it’s unnecessary suffering.
Don’t let misinformation keep you from proper care. Opioid nausea is treatable. You just need the right tools.
Final Thoughts
Opioid-induced nausea isn’t a sign you’re doing something wrong. It’s a predictable side effect with proven solutions. You don’t have to suffer through it. Use low-dose initiation, time your antiemetics before your opioid, eat simple meals, and don’t hesitate to switch opioids if needed. Most people find relief within a week. And if you do, you’ll be able to take your pain medicine without fear-and live better while you do.How long does opioid-induced nausea last?
For most people, nausea from opioids lasts 3 to 7 days after starting or increasing the dose. After that, the body usually builds tolerance. If nausea continues beyond a week despite treatment, it’s time to reassess your medication or dosing strategy.
Can I take ginger with my opioid and antiemetic?
Yes. Ginger (250-500 mg in capsule form or as tea) is safe to use alongside opioids and antiemetics like haloperidol or metoclopramide. It’s not a replacement for medication, but studies show it can help reduce nausea severity, especially when paired with dietary changes.
Is it safe to stop my antiemetic after a few days?
Yes-if your nausea has fully resolved and you’ve been on a stable opioid dose for at least 5-7 days. Don’t stop abruptly if you’re still feeling sick. But once tolerance kicks in, you can safely discontinue the antiemetic. No rebound nausea is expected.
Why does my nausea get worse when I eat?
Opioids slow stomach emptying, so food sits longer and can trigger nausea. This is especially true with heavy or greasy meals. Eating small, bland portions and staying upright after eating helps. If constipation is also an issue, treating that often improves nausea too.
Can I switch from morphine to oxycodone myself?
No. Switching opioids requires careful dose conversion to avoid overdose or withdrawal. Morphine and oxycodone aren’t interchangeable on a 1:1 basis. Always work with your doctor or pharmacist to make this change safely.
What to Do Next
If you’re struggling with opioid nausea right now:- Check your current opioid dose. Is it higher than recommended for someone new to opioids? If so, ask about lowering it by 25-33%-many people keep good pain relief with less.
- Review your antiemetic timing. Are you taking it before or after your opioid? Adjust to 30-60 minutes before.
- Start eating smaller, bland meals and avoid eating within an hour of taking your pain pill.
- Write down when nausea happens and what you ate or did before it started. Bring this to your next appointment.
- If none of this helps after 5 days, ask about switching to hydromorphone or methadone.
You don’t have to choose between pain relief and feeling sick. With the right approach, you can have both.


12 Comments
OMG this is LIFE-SAVING info 😭 I was about to quit my pain meds until I read this. Ginger tea + taking my haloperidol at 7am before my oxycodone at 8am? Game changer. My stomach actually stopped rebelling. Thank you so much for this 🙏✨
The empirical basis for timing antiemetics 30–60 minutes prior to opioid administration is well-supported in pharmacokinetic literature. The Cmax of most oral opioids occurs between 60 and 90 minutes post-ingestion; thus, pre-emptive pharmacological intervention aligns with peak plasma concentration dynamics. This is not anecdotal-it is clinical pharmacology applied correctly.
Haloperidol? Really? That’s like using a sledgehammer to crack a walnut… And you’re suggesting people just… take it? Without monitoring QT intervals? Or considering extrapyramidal side effects? I suppose you also recommend giving aspirin to toddlers for fevers…
And ginger? As if that’s some magical herb from the Himalayas… Please. This is not a wellness blog. This is medicine.
I appreciate the thoroughness of this post-but I must say, the fact that so many patients are left to suffer through this preventable side effect speaks to a systemic failure in pain management education. I’ve seen elderly patients abandon opioids entirely because no one told them about timing or ginger. This isn’t just clinical-it’s ethical. Thank you for writing this.
Wow. So you’re telling me… you can actually *think* your way out of nausea? Like, you just… *time* your pills? And eat toast? And use GINGER? I’m crying. I’ve been taking 80mg of oxycodone daily for 3 years and I thought I was just a weakling. Turns out I just didn’t have a Pinterest board.
Next you’ll tell me sunlight cures depression and water hydrates you. What’s next? Maybe you can explain why gravity exists? 😏
THIS. IS. EVERYTHING. I’ve been on morphine for 8 months. Nausea was killing me. I tried everything-Zofran, Dramamine, even CBD gummies (don’t judge me). Nothing. Then I read this. Took my haloperidol at 6:30am, had a cracker at 8:30am, stayed upright. And guess what? I didn’t throw up for 3 days straight. I cried. I actually cried. This isn’t just advice-it’s redemption.
Also, switching to hydromorphone? I did it. My doctor laughed. Now he’s asking me how I did it. I sent him this post. He’s now recommending it to his other patients. Thank you. From the bottom of my gut.
The data presented here is methodologically sound and clinically relevant. The emphasis on individualized timing and avoidance of prophylactic polypharmacy reflects current best practices in palliative care. The omission of cost-effectiveness analysis is minor, as the inclusion of generic alternatives demonstrates pragmatic awareness. This is a model for patient-centered education.
bro u just said take haloperidol like its candy?? that shit makes u feel like ur robot from the matrix 😭 and ginger? lmao my grandma uses that for seasickness. u think i’m gonna chug tea while my pain meds hit?? nah fam. i just take zofran and pray. also who the fuck is this guy that wrote this like he’s a doctor??
Let me guess-this was written by Big Pharma, right? Haloperidol is cheap… because it’s been around since the 1950s. They don’t want you to know that the FDA has quietly suppressed studies linking opioid nausea to neurotoxicity from long-term use. And ginger? A natural remedy that Big Medicine can’t patent. They’d rather you take five different pills than one herb. Wake up.
Also, why is no one talking about the fact that opioid-induced nausea is often a sign your body is detoxing from sugar and processed foods? Maybe you’re not sick from morphine… you’re sick from McDonald’s.
Oh please. You’re telling me that if I just eat toast and wait 7 days, I won’t feel sick? I’ve been on oxycodone for 10 years. I’ve tried every antiemetic known to man. My stomach still feels like it’s hosting a rave. This is a scam. You’re just giving people false hope. I’ve seen this before-some ‘expert’ writes a blog and suddenly everyone thinks they’re a neurologist. Newsflash: not everyone adapts. Some of us just have to live with it.
just tried the 30 min before trick and holy crap it worked. i was gonna quit my meds. now i’m actually sleeping. also ginger tea is kinda nice. thanks for not being a doctor who just shrugs and says ‘it’ll pass’.
So… you’re saying the entire opioid system is designed to make you sick so you’ll keep taking pills? And they’re selling you ginger as a ‘supplement’ because it’s cheaper than real treatment? I’ve been researching this for months. This isn’t medicine-it’s control. They want you dependent. Haloperidol? That’s a psychiatric drug. They’re masking symptoms to keep you compliant. I’m not taking it.
Also, the FDA is in bed with pharma. And your ‘low-dose start’? That’s just to get you hooked slower. They don’t want you to quit. They want you addicted. You think this is helpful? It’s manipulation.