Anticoagulant Side Effects: What You Need to Know Before Taking Blood Thinners
When you take an anticoagulant, a medication that prevents blood clots by slowing down the clotting process. Also known as blood thinners, these drugs are life-saving for people with atrial fibrillation, deep vein thrombosis, or artificial heart valves—but they come with risks you can’t ignore. The biggest concern? bleeding. It’s not just a minor bruise. Anticoagulants can cause dangerous internal bleeding, even from small injuries, because your blood can’t clot the way it should. That’s why knowing the signs isn’t optional—it’s essential.
These drugs don’t work the same way. Warfarin, apixaban, rivaroxaban, and dabigatran all target different parts of the clotting system, and each has its own set of side effects. Warfarin requires regular blood tests and strict diet control because it reacts with vitamin K in leafy greens. Newer ones like apixaban don’t need monitoring, but they still carry a risk of serious bleeding, especially if you’re also taking NSAIDs like ibuprofen or aspirin. And here’s something most people don’t realize: even a minor fall or head bump can turn dangerous when you’re on an anticoagulant. That’s why many doctors advise avoiding contact sports or high-risk activities.
It’s not just about bleeding. Some people report fatigue, nausea, or skin rashes. Others develop hair loss or purple toes syndrome—a rare but painful reaction tied to cholesterol crystals blocking small vessels. And if you’re scheduled for surgery, dental work, or even a cosmetic procedure like Botox or laser treatment, stopping your anticoagulant isn’t always the answer. In fact, stopping can be riskier than continuing, especially if you’re at high risk for clots. That’s why you need to talk to your doctor before any procedure, not just your surgeon or dentist.
Drug interactions are another silent threat. Antibiotics, antifungals, and even some herbal supplements like St. John’s wort can make anticoagulants stronger or weaker overnight. A single new prescription could push your INR into dangerous territory. That’s why keeping a full list of everything you take—including over-the-counter meds and vitamins—isn’t just good practice, it’s a safety must.
And don’t assume you’re safe just because you feel fine. Many people don’t notice internal bleeding until it’s too late. Watch for unusual bruising, pink or red urine, black or tarry stools, severe headaches, or sudden weakness on one side of your body. These aren’t normal. They’re red flags.
Below, you’ll find real-world advice from people who’ve lived with these drugs. You’ll learn how to reduce bruising during cosmetic procedures, how to spot hidden interactions, and what to do when side effects hit. This isn’t theory—it’s what works for real patients trying to stay safe while staying healthy.
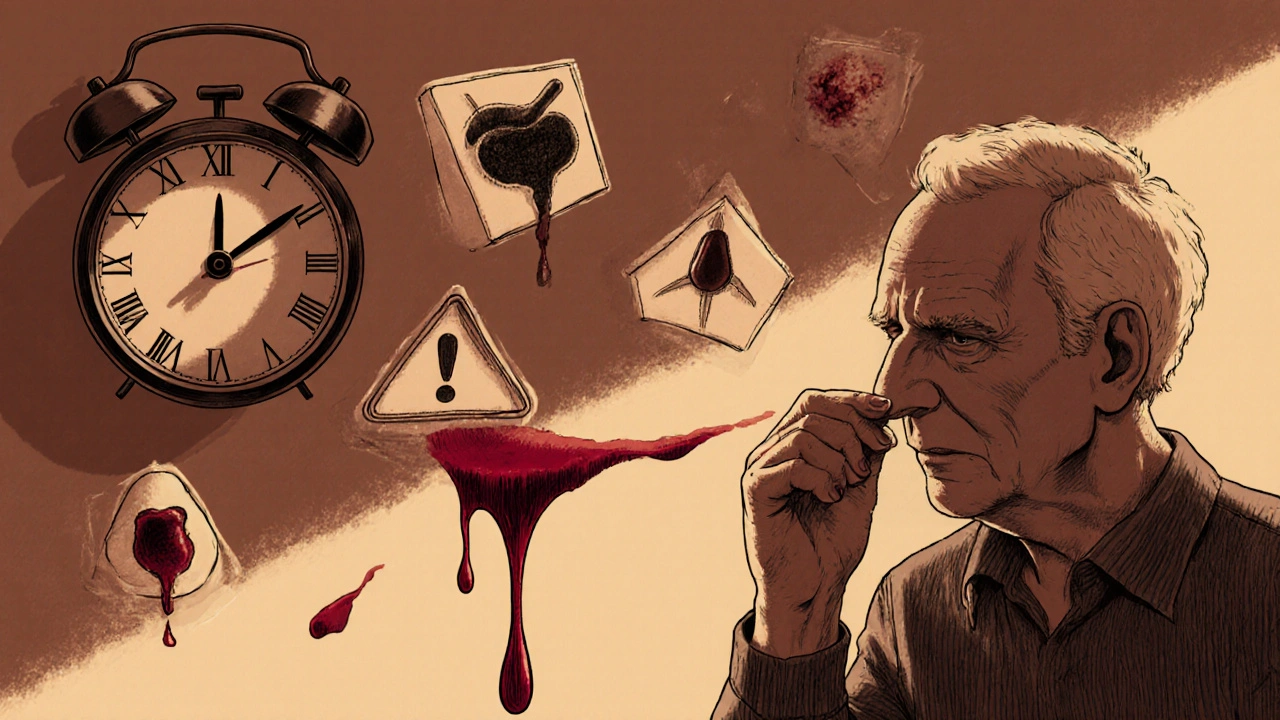
Severe Bleeding on Medications: What to Watch For and How to Respond in an Emergency
Severe bleeding from blood thinners is a silent threat that kills. Learn the warning signs, who’s most at risk, what happens in the ER, and how to protect yourself before it’s too late.
read more
