Steroid-Induced Osteoporosis Risk Calculator
Personal Information
Lifestyle Factors
Key Recommendations
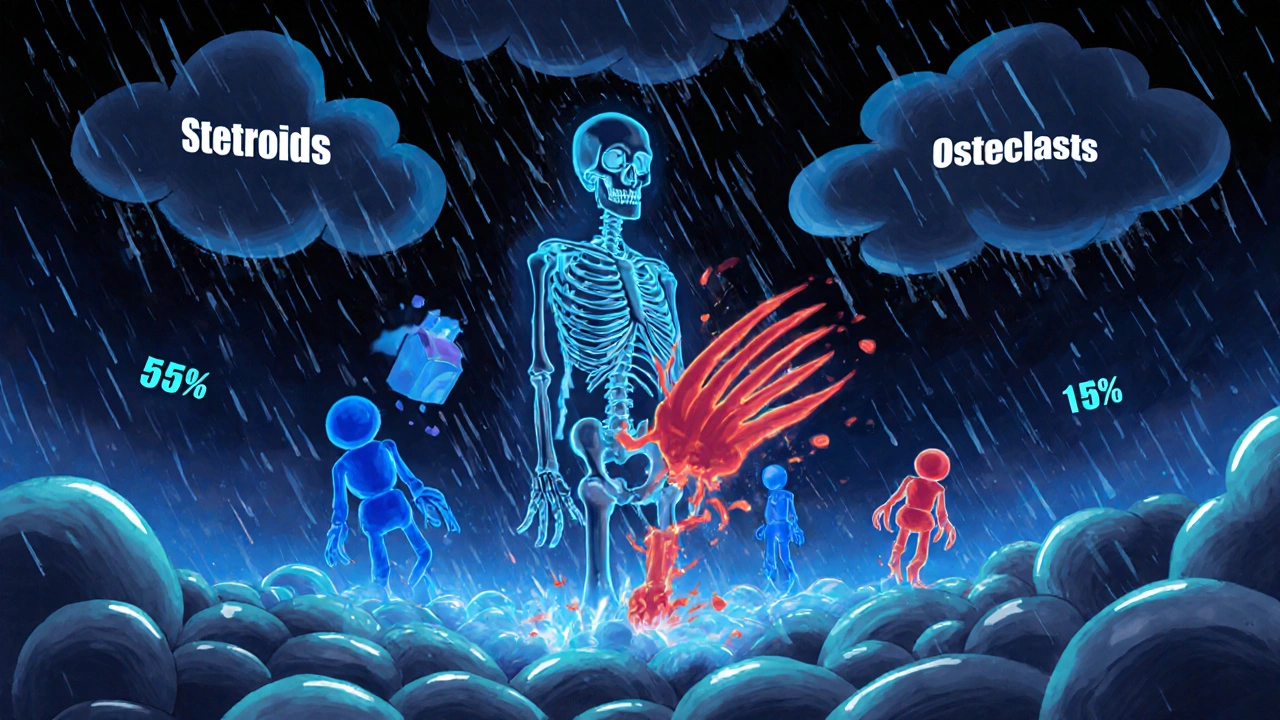
Most patients on steroids: Only 15% receive full guideline-recommended care.
Most important action: Get a bone density scan (DXA) right after starting steroids.
Why Long-Term Steroids Put Your Bones at Risk
When you take steroids like prednisone for months or years - whether for arthritis, lupus, asthma, or another autoimmune condition - your bones start breaking down faster than they can rebuild. This isn’t just a side effect. It’s a direct, well-documented medical problem called glucocorticoid-induced osteoporosis (GIOP). Within just 3 to 6 months of starting daily steroids, your fracture risk jumps by 70% to 100%. That’s not a slow, creeping danger. It’s a silent storm that hits fast.
Studies show that bone mineral density (BMD) drops 5% to 15% in the first year, especially in the spine. Even low doses matter. If you’re taking 2.5 mg of prednisone or more every day for three months or longer, you’re already in the high-risk group. At 7.5 mg or higher, your fracture risk doubles. And here’s the kicker: every extra milligram of daily steroid reduces your spine BMD by 1.4% per year. That’s not theoretical. That’s measurable, real-world data.
How Steroids Attack Your Bones
Steroids don’t just make you gain weight or cause mood swings. They mess with your bones at the cellular level. They shut down the cells that build bone - osteoblasts - and speed up the cells that break it down - osteoclasts. This imbalance means your skeleton is losing more than it’s gaining. Your body also absorbs less calcium from food, leaks more calcium through your kidneys, and becomes less responsive to the bone-strengthening effects of walking or lifting weights.
One study found that steroids reduce your bones’ ability to respond to physical activity by about 25%. So even if you’re trying to stay active, the steroids are working against you. This isn’t about being lazy. It’s about biology. Your bones are under chemical siege.
The First Line of Defense: Dose and Duration
The most powerful tool you have is also the simplest: take the lowest dose for the shortest time possible. This isn’t advice from a distant doctor. It’s backed by hard numbers. When patients cut their daily steroid dose from over 7.5 mg down to 7.5 mg or less, their fracture risk dropped by 35% in just six months.
That means if you’re on 10 mg a day, talk to your doctor about whether you can drop to 7.5 mg. If you’re on 15 mg, can you get to 10 mg? Every reduction counts. This isn’t about stopping treatment - it’s about finding the minimum effective dose. Many patients stay on high doses longer than needed because they’re afraid symptoms will return. But with careful monitoring, dose reduction is often possible without flare-ups.
Calcium and Vitamin D: Non-Negotiable Basics
Every single person on long-term steroids needs calcium and vitamin D. No exceptions. The numbers are clear: aim for 1,000 to 1,200 mg of calcium daily. Get as much as you can from food - dairy, leafy greens, fortified foods - then fill the gap with supplements. For vitamin D, 600 to 800 IU is the minimum. Many experts recommend 800 to 1,000 IU to ensure your blood levels stay above 20 ng/mL.
Why? Because without enough vitamin D, your body can’t absorb calcium. And without enough calcium, your bones have nothing to rebuild with. A major study showed that people taking 1,000 mg calcium and 500 IU vitamin D daily lost only 0.72% of spine BMD per year. Those on placebo lost 2% - nearly three times faster. This isn’t a luxury. It’s your foundation.

Movement Matters - Even With Steroids
You don’t need to run marathons. You need to move regularly. Weight-bearing exercise - walking, stair climbing, dancing, light weight training - tells your bones to stay strong. Aim for at least 30 minutes most days. Even standing more throughout the day helps. But don’t expect miracles. Steroids blunt your bones’ response to movement by about a quarter. So you need to be more consistent than someone not on steroids.
And don’t skip the balance work. Falls are a leading cause of fractures in older adults, and steroid users are at higher risk. Simple exercises like standing on one foot for 30 seconds, heel-to-toe walking, or tai chi can reduce fall risk. It’s not glamorous. But it’s protective.
Quit Smoking, Limit Alcohol
Smoking doesn’t just hurt your lungs - it kills bone density. Smokers on steroids have a 25% to 30% higher fracture risk than non-smokers. Quitting doesn’t just help your lungs. It helps your spine, hips, and wrists. Alcohol is equally damaging. More than three drinks a day increases fracture risk. Stick to one or two at most. And if you’re drinking daily, talk to your doctor. This isn’t about willpower. It’s about survival.
When Medication Becomes Necessary
Calcium and vitamin D aren’t enough for everyone. If you’re on steroids long-term and have other risk factors - like being over 50, having a prior fracture, or a family history of osteoporosis - you likely need stronger help. The first-line drug? Bisphosphonates. Risedronate (5 mg daily or 35 mg weekly) cuts vertebral fracture risk by 70%. Alendronate works too. Zoledronic acid, given as an annual IV infusion, boosts spine BMD by 4.5% in a year - far more than placebo.
For those with severe bone loss (T-score of -2.5 or worse) or a history of fractures, teriparatide is the most powerful option. It’s a daily injection that stimulates new bone growth. Studies show it increases spine BMD by 9.1% in 12 months - nearly double the gains of bisphosphonates. Denosumab, given as a shot every six months, is another strong alternative, adding 7% to spine density.
These aren’t optional. If your doctor hasn’t mentioned them, ask. Many patients assume osteoporosis is just part of aging. It’s not. It’s preventable.

The Stark Reality: Most People Get No Protection
Here’s the ugly truth: only 15% of people on long-term steroids get full, guideline-recommended care. Only 31% have had a bone density scan. Only 40% are documented as taking calcium. Only 37% are getting vitamin D. Men are far less likely than women to be screened - 44% vs 76%. That’s not just negligence. It’s systemic failure.
Why? Because doctors don’t always talk to each other. A rheumatologist might know you’re on steroids, but your primary care doctor doesn’t. Patients think bone loss is inevitable. They’re told, “Just take your pills,” but never told, “Your bones are at risk.” And pharmacies don’t track who needs what.
How to Take Control
You can’t fix this alone, but you can demand better care. Here’s your action plan:
- Ask your doctor for a bone density scan (DXA) as soon as you start long-term steroids - not in a year, not next year. Now.
- Get your vitamin D level checked. If it’s under 30 ng/mL, you need more.
- Write down your steroid dose. Know if you’re above or below 2.5 mg/day.
- Ask: “Am I at high risk for fractures? Do I need a bone-building drug?”
- Request a referral to a pharmacist who specializes in osteoporosis prevention. Pharmacist-led programs have boosted proper care from 35% to 85% in real clinics.
- Set phone reminders for your calcium and vitamin D. Adherence drops to 40% after a year - not because people don’t care, but because they forget.
What Happens If You Do Nothing?
Half of all steroid-related fractures happen in the first year. A spinal fracture can mean chronic pain, loss of height, difficulty breathing, and a lifetime of disability. A hip fracture often means surgery, months of rehab, and a 20% higher chance of dying within a year. This isn’t fear-mongering. It’s statistics. And it’s preventable.
Final Thought: Prevention Starts Day One
The best time to protect your bones was when you started steroids. The second-best time is today. You don’t need to be perfect. You just need to be consistent. Take your calcium. Move every day. Ask the hard questions. Push for the scan. Demand the right meds. Your bones can’t speak for themselves. But you can. And you should.
Can you reverse steroid-induced osteoporosis?
Yes, to a significant degree. While lost bone isn’t fully restored, medications like teriparatide and denosumab can rebuild bone density by 7% to 9% in the spine within a year. Bisphosphonates stop further loss and may slightly improve density. The key is early intervention - the longer you wait, the harder it is to recover.
Do all steroids cause bone loss?
Only systemic steroids - those taken orally, by injection, or IV - cause significant bone loss. Topical creams, inhalers, or nasal sprays used for asthma or eczema rarely affect bones because they don’t reach high enough levels in the bloodstream. But if you’re taking prednisone, methylprednisolone, or similar pills for months, your bones are at risk.
How often should I get a bone scan if I’m on steroids?
Get your first scan right after starting long-term steroid therapy. Then repeat every 1 to 2 years if you’re still on steroids. If you start a bone-building drug, get another scan after 12 months to see if it’s working. Some patients need more frequent testing if their dose is high or their BMD is very low.
Can I stop taking steroids to protect my bones?
Never stop steroids suddenly. Doing so can trigger life-threatening adrenal crisis. But you can work with your doctor to reduce your dose to the lowest level that controls your condition. Many people can taper safely over weeks or months. The goal isn’t to quit steroids if you need them - it’s to use the least amount possible for the shortest time.
Are there natural alternatives to bisphosphonates?
No. While calcium, vitamin D, exercise, and quitting smoking help, they are not enough on their own for moderate to high-risk patients. There are no proven herbal or supplement alternatives that match the fracture-reducing power of bisphosphonates, denosumab, or teriparatide. Relying on “natural” remedies alone puts you at serious risk of fractures.
Why do men get less screening for steroid osteoporosis?
There’s a deep bias in medicine that osteoporosis is a “woman’s disease.” But men on long-term steroids lose bone just as fast - and often with worse outcomes. Men are less likely to be screened because providers assume they’re at lower risk. But data shows men on steroids have a fracture risk equal to women of the same age and dose. This gap needs to be addressed by both doctors and patients.
What if I can’t afford the bone meds?
Many bisphosphonates like alendronate and risedronate are available as low-cost generics under $10 a month. Zoledronic acid infusions may be covered by insurance if you meet criteria. Ask your doctor about patient assistance programs, pharmacy discount cards, or manufacturer coupons. Never skip treatment because of cost - the cost of a hip fracture is far higher, both financially and physically.


14 Comments