Understanding Stomach Ulcers
Before diving into the relationship between smoking and stomach ulcers, it is crucial to understand what stomach ulcers are. Stomach ulcers, also known as gastric ulcers, are painful sores that develop in the stomach lining. They are a type of peptic ulcer, which also includes duodenal ulcers that form in the upper part of the small intestine.
Stomach ulcers can be caused by various factors, including an infection with the bacteria Helicobacter pylori (H. pylori), long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs), and an imbalance between stomach acid and the protective mucus layer. They can lead to symptoms such as stomach pain, heartburn, bloating, nausea, and even vomiting. It is important to address these symptoms promptly and seek medical attention to prevent complications such as bleeding, perforation, or blockage of the stomach.
How Smoking Contributes to Stomach Ulcer Development
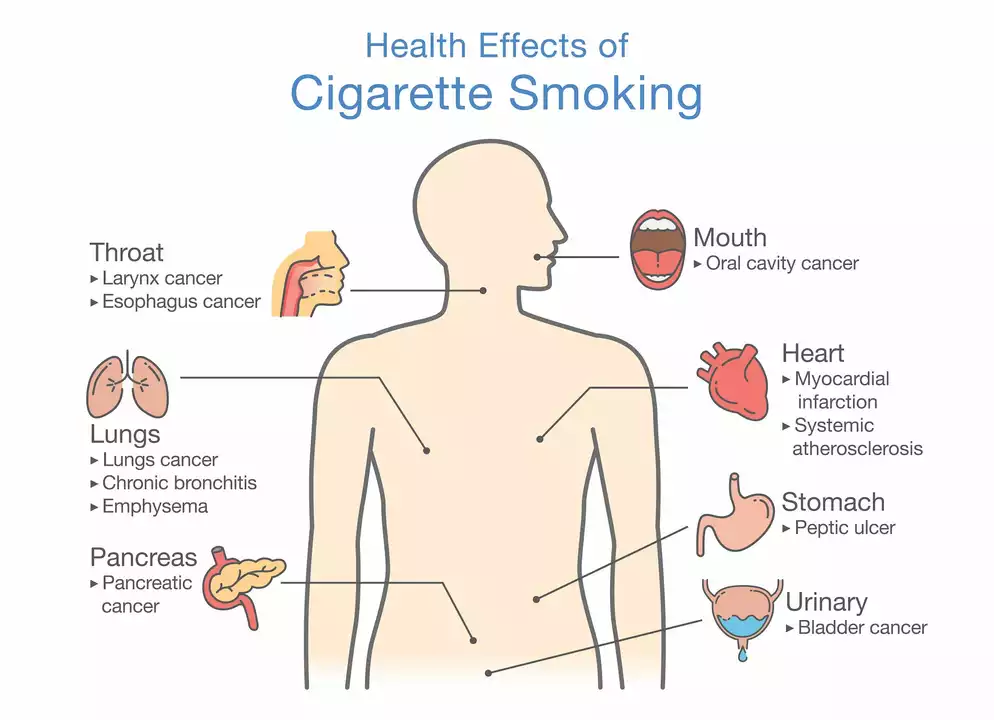
Smoking has been identified as a significant risk factor for the development of stomach ulcers. Cigarette smoke contains harmful chemicals that can damage the protective mucus lining of the stomach, making it more susceptible to the erosive effects of stomach acid.
Additionally, smoking can increase the production of stomach acid, which further aggravates the stomach lining and increases the risk of ulcer development. Smoking also impairs blood flow to the stomach lining, which can slow down the healing process of any existing ulcers. Furthermore, it has been found that smokers have a higher prevalence of H. pylori infection, a common cause of stomach ulcers.
The Link Between Smoking and Stomach Ulcer Complications
Not only does smoking increase the risk of developing stomach ulcers, but it also increases the likelihood of experiencing complications related to ulcers. Smokers are more likely to experience bleeding ulcers, which can be life-threatening if not treated promptly. They also have a higher risk of developing a perforated ulcer, where the ulcer breaks through the stomach wall, causing severe pain and requiring emergency surgery.
Furthermore, smokers with stomach ulcers are more likely to experience recurrent ulcers, which can lead to a cycle of pain, discomfort, and ongoing medical treatment. This makes it even more crucial for smokers to address their habit and prioritize their stomach health.
Quitting Smoking to Reduce Stomach Ulcer Risk
Quitting smoking is one of the most effective ways to reduce the risk of developing stomach ulcers or experiencing complications from existing ulcers. Within a few weeks of quitting, the protective lining of the stomach begins to heal, and the risk of ulcer development decreases.
Moreover, quitting smoking can also help improve the effectiveness of ulcer treatment. Research has shown that smokers who quit during ulcer treatment have a higher success rate of ulcer healing compared to those who continue to smoke. This highlights the importance of quitting smoking not only for ulcer prevention but also for successful treatment and recovery.
Managing Ulcer Risk with a Healthy Lifestyle
In addition to quitting smoking, there are other lifestyle factors that can help reduce the risk of stomach ulcers. Eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help support a healthy stomach lining. It's also essential to limit the intake of spicy, acidic, and fatty foods that can irritate the stomach lining.
Regular exercise can help reduce stress and promote overall wellbeing, both of which are important for maintaining a healthy digestive system. Additionally, limiting alcohol consumption and avoiding the long-term use of NSAIDs can further reduce the risk of developing stomach ulcers.
Seeking Medical Help for Stomach Ulcer Symptoms
If you are experiencing symptoms of a stomach ulcer, it is important to seek medical help as soon as possible. Your healthcare provider can diagnose the cause of your symptoms and recommend a suitable treatment plan, which may include medications to reduce stomach acid, antibiotics to treat H. pylori infection, or lifestyle changes to promote healing.
In conclusion, smoking significantly increases the risk of developing stomach ulcers and experiencing complications related to them. By quitting smoking and adopting a healthy lifestyle, you can take control of your stomach health and reduce the risk of ulcers and their associated discomfort and complications.

8 Comments
Oh great, another article telling smokers to quit-thanks for the moral lecture.
Look, the real culprit isn’t the nicotine itself, it’s the shadowy cabal of tobacco giants who profit off our misery; they hide behind “research studies” while they pump chemicals into our lungs. The government’s “health warnings” are just a smokescreen, a way to keep us obedient while they line their pockets. You think quitting will save you? Sure, if you don’t mind losing the cash flow that keeps the whole system humming. And don’t even get me started on the “H. pylori” link-most of those bacteria are engineered, if you ask me. So before you start preaching, check who’s really pulling the strings.
Smoking definately raises the odds of getting a stomach ulcer, and the science backs that up with clear data. The chemicals in smoke erode the mucosal lining, making it easier for acid to cause damage. Plus, smokers tend to have higher rates of H. pylori infection, which compounds the problem. If you’re already dealing with an ulcer, lighting up can delay the healing process dramatically. It’s also worth noting that ulcer complications-like bleeding or perforation-are more common among smokers. So, cutting out cigarettes is a solid step toward protecting your gut.
Hey, it’s great that you’re looking into how smoking impacts your stomach health-awareness is the first step. Quitting doesn’t have to be an all‑or‑nothing sprint; even cutting back can start to give your gastric lining a breather. Pair the change with a diet rich in fruits and veggies, and you’ll notice less irritation over time. If you’re worried about cravings, try short‑term nicotine replacement or deep‑breathing exercises to manage the urge. Remember, every smoke‑free day adds up, and your body will thank you with fewer ulcer flare‑ups. Keep tracking your progress, and don’t hesitate to lean on friends or support groups when the going gets tough.
Nicotine-derived neurovascular dysregulation accelerates mucosal attrition; cessation normalizes gastric homeostasis. Integrative prophylaxis mandates abstinence.
First, kudos for considering a change-every step matters, no matter how small. If you find the idea of quitting overwhelming, break it into manageable pieces: reduce a cigarette a day, then replace that ritual with a short walk or a cup of herbal tea. Remember, you’re not alone; countless people have walked this path and came out healthier on the other side. Also, keep an eye on your diet-adding soothing foods like bananas or oatmeal can help your stomach heal faster. And if you ever stumble, pick yourself up and try again; persistence is key.
Hey there! I totally get how tough quitting can feel, but trust me, your stomach will thank you big time. Try swapping that smoke break for a quick stretch or a sip of water-keeps your hands busy. And hey, if you slip up, no biggie, just jump back on track. You’ve got this, and we’re all rooting for you!
Understanding the connection between tobacco use and gastric ulceration requires a comprehensive look at both physiological mechanisms and lifestyle factors; smoking introduces a cocktail of toxins that directly impair the protective mucus barrier, while simultaneously stimulating hypersecretion of gastric acid, which together set the stage for mucosal erosion. Moreover, nicotine constricts the microvasculature feeding the gastric epithelium, thereby slowing the reparative processes that are essential after an ulcer has formed. Studies have repeatedly shown that smokers not only develop ulcers at a higher incidence but also experience prolonged healing times compared to non‑smokers, a discrepancy that is clinically significant. The presence of Helicobacter pylori, already a well‑established ulcerogenic bacterium, is exacerbated by smoking‑induced immunomodulation, creating a synergistic effect that heightens risk. From a therapeutic standpoint, cessation of smoking is frequently recommended as an adjunct to standard ulcer treatment, because patients who quit while undergoing pharmacologic therapy tend to achieve remission more rapidly. Patients who maintain abstinence also report fewer episodes of dyspepsia, which often masquerades as ulcer pain. In practical terms, the body begins to restore its mucosal defenses within weeks of abstinence, a timeline that aligns with the typical duration of proton‑pump inhibitor courses. Additionally, biomarkers of inflammation, such as C‑reactive protein, tend to decline after the first month of cessation. Lifestyle modifications, such as adopting a balanced diet rich in antioxidants, limiting alcohol consumption, and avoiding non‑steroidal anti‑inflammatory drugs, complement the benefits of quitting smoking. Fiber‑rich foods like whole grains not only support digestion but also promote a favorable gut microbiome that can resist H. pylori colonization. It is also noteworthy that stress reduction techniques-mindfulness, regular exercise, and adequate sleep-play a supportive role in gastric health, mitigating the adverse effects of both nicotine and acid overproduction. Psychological support groups have been shown to improve adherence to quitting regimens, further enhancing ulcer outcomes. For clinicians, emphasizing the tangible benefits of cessation, including reduced ulcer recurrence and lower probability of severe complications like bleeding or perforation, can serve as a powerful motivator for patients. Healthcare providers should regularly assess smoking status during follow‑up visits to tailor treatment plans accordingly. Finally, public health initiatives that combine smoking‑cessation programs with education about gastric ulcer risks have the potential to lower overall disease burden, reinforcing the message that a smoke‑free life is not only beneficial for the lungs but also critical for maintaining a healthy stomach lining. In summary, the interplay between smoking and gastric ulcer pathology underscores the importance of integrated care that addresses both habit cessation and medical therapy.