Understanding Contraception and Cancer Risk
As a blogger who cares about health and well-being, I feel it's essential to discuss the connection between contraception and cancer risk. This article will delve into various aspects of this topic, aiming to provide you with comprehensive information to help you make informed decisions about your reproductive health.
A Brief Overview of Contraceptive Methods
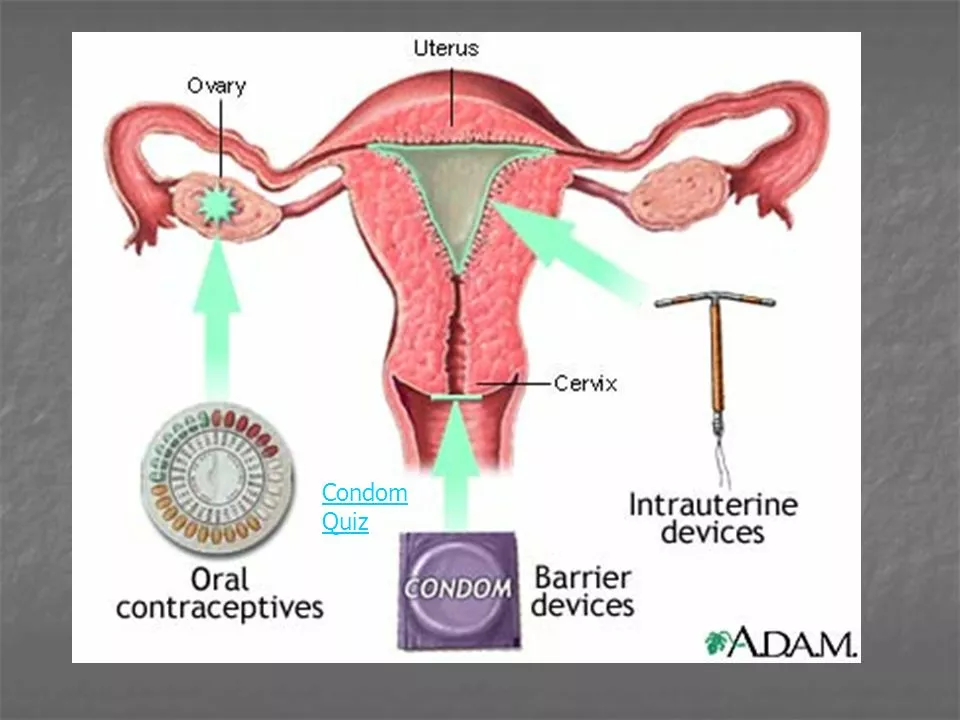
Before we dive into the connection between contraception and cancer risk, let's first understand the different contraceptive methods available. There are several types of contraceptives, including barrier methods (condoms, diaphragms), hormonal methods (birth control pills, patches, vaginal rings, injections, and hormonal IUDs), and intrauterine devices (IUDs).
Each method has its advantages and disadvantages, and you should choose the one that works best for you and your lifestyle. However, it's essential to be aware of the potential risks associated with each method, including the potential for increased cancer risk.
Oral Contraceptives and Cancer Risk
Oral contraceptives, commonly known as birth control pills, are a popular method of hormonal contraception. Several studies have explored the relationship between the use of oral contraceptives and an increased risk of certain types of cancer. Some research suggests that long-term use of oral contraceptives may increase the risk of developing breast, cervical, and liver cancer.
However, it's essential to note that other studies have found no significant association between oral contraceptives and cancer risk. Additionally, some research has even found that using birth control pills may reduce the risk of developing ovarian and endometrial cancer.
Hormonal Injections and Cancer Risk
Hormonal injections, such as Depo-Provera, are another form of hormonal contraception that has been studied for its potential link to cancer risk. Some studies have found an increased risk of breast cancer among women who have used hormonal injections, particularly those who used them for an extended period.
However, similar to oral contraceptives, research on hormonal injections and cancer risk is not unanimous, and some studies have found no significant association. More research is needed to fully understand the relationship between hormonal injections and cancer risk.
The IUD and Cancer Risk
Intrauterine devices (IUDs) are a long-term, reversible form of contraception. There are two main types of IUDs: hormonal and non-hormonal (copper). Some studies suggest that hormonal IUDs may slightly increase the risk of breast cancer. However, this risk appears to be relatively small and may decrease after discontinuing the use of the IUD.
Non-hormonal IUDs, such as the copper IUD, have not been associated with an increased risk of cancer. In fact, some research suggests that the copper IUD may even provide some protection against endometrial cancer.
Barrier Methods and Cancer Risk
Barrier methods of contraception, such as condoms and diaphragms, have not been associated with an increased risk of cancer. In fact, using condoms consistently and correctly can help protect against sexually transmitted infections (STIs), including human papillomavirus (HPV), which is a primary cause of cervical cancer.
While barrier methods do not have a direct effect on cancer risk, they play a crucial role in overall reproductive health by preventing the spread of STIs.
Contraception and Cancer Risk: The Bigger Picture
It's essential to consider the overall context when discussing the connection between contraception and cancer risk. Many factors contribute to a person's risk of developing cancer, including genetics, lifestyle choices, and exposure to environmental toxins. Contraceptive use is just one piece of the puzzle, and it's crucial to weigh the benefits and risks of each method for your individual situation.
Moreover, it's important to remember that effective contraception can help prevent unintended pregnancies, which can have significant implications for a person's physical, mental, and emotional well-being.
Discussing Contraception and Cancer Risk with Your Healthcare Provider
If you have concerns about the relationship between contraception and cancer risk, it's essential to discuss them with your healthcare provider. They can provide personalized advice based on your medical history, risk factors, and contraceptive needs. Your healthcare provider can also help you weigh the benefits and risks of different contraceptive methods and help you choose the best option for your unique circumstances.
Conclusion
Understanding the connection between contraception and cancer risk is essential for making informed decisions about your reproductive health. While some studies have suggested a potential link between certain types of contraceptives and an increased risk of specific cancers, the overall risk is generally small and must be weighed against the benefits of effective contraception. Consult with your healthcare provider to discuss your concerns and find the best contraceptive method for your individual needs.






13 Comments
I've been digging into the estrogenic modulation associated with combined oral contraceptives, and the data suggests a nuanced carcinogenic risk profile that can't be dismissed outright.
While some epidemiological cohorts flag a marginal uptick in breast neoplasm incidence, the confidence intervals often overlap with baseline population figures.
Moreover, the protective effect against ovarian and endometrial malignancies appears statistically robust across multiple meta‑analyses.
Thus, clinicians should weigh both oncologic and reproductive outcomes when counseling patients, rather than resorting to blanket statements.
In practice, individualized risk assessment remains the gold standard.
Great summary, really helped me see the bigger picture! 😊
Yo folks, lemme break down what this whole contraception‑cancer thing really looks like in everyday life. First off, you gotta realize that hormones in birth control pills act like little signal boosters for your body's own estrogen pathways, and that can sometimes give cancer cells a bit of a leg up. 📈 But hold up – the same hormonal cocktail also shuts down the ovary's egg‑making machinery, which can actually lower your odds of getting ovarian cancer in the long run. 🥚 No joke, that trade‑off is why docs often say the benefits outweigh the risks for most peeps. Then there’s the patch and the ring – they sorta deliver hormones more steadily, which might mean less spikes that could trigger cell growth, but the research is still kinda fuzzy on that. 💊 When you look at injections like Depo‑Provera, the data shows a slight bump in breast cancer stats, especially if you stay on it for years, but it’s still debated whether that’s a causal link or just a correlation. 🤔 Also, don't forget the IUDs – hormonal IUDs dump a local dose of progestin that can mildly raise breast cancer numbers, yet they also protect against endometrial cancer, which is a pretty sweet side‑effect. 🌟 The copper IUD? Totally non‑hormonal, and some studies even hint it might guard against certain uterine cancers, so that’s a win for folks who wanna stay clear of hormones. 👏 Barrier methods like condoms don’t raise any cancer flags and actually cut down HPV transmission, which is a big deal because HPV is a major driver of cervical cancer. 🎯 So, in a nutshell, every method has its own risk‑benefit calculus, and the overall increase in cancer risk is generally small compared to the huge reproductive health benefits. 🤓 Bottom line: chat with your healthcare provider, look at your personal and family medical history, and pick the tool that feels right for you. 💡 Remember, staying informed and proactive is the best defense against any potential health hiccup. 🙌 Lastly, keep an eye on new research – the science is always evolving, and what we know today might be tweaked tomorrow. 🚀 Anyway, hope this clears things up a bit, and stay safe out there!
The evidence demonstrates that hormonal contraceptives modestly elevate breast cancer incidence while concurrently reducing ovarian and endometrial cancer risk.
Healthcare professionals must prioritize evidence‑based counseling, emphasizing both the quantitative risk increments and the protective benefits.
Patients should be empowered to make informed choices, not swayed by sensationalized claims.
When we step back from the headlines, the interplay between reproductive autonomy and oncologic risk mirrors a broader dialectic about control over one's body versus the inevitabilities of biology.
Each contraceptive choice is a micro‑decision that reverberates through personal health narratives, reflecting both societal pressures and individual agency.
Understanding this nuance invites us to consider not just statistical probabilities, but the lived experiences behind those numbers.
It's reassuring to see the non‑hormonal options highlighted, especially for those wary of hormonal side‑effects. 😊 Keeping the conversation balanced helps everyone feel seen.
The hormonal IUD's subtle influence on breast tissue can feel like a silent alarm you never heard coming. Yet many women live blissfully unaware.
Hey everyone, just wanted to add that talking openly with your doctor can turn what feels like a confusing maze into a clear path.
They can tailor advice to your unique genetic background and lifestyle, making sure you’re comfortable with the benefits and any potential risks. 😊
Contraception choices reflect personal values and health goals they shape lives each day not just stats but stories we live with each decision you pick what feels right for you
Imagine your body as a vibrant garden; hormonal pills are like a gentle rain that nurtures certain blossoms while maybe giving a few weeds a chance to sprout – the key is knowing which seeds you want to flourish and which to prune.
I appreciate the balanced overview; it's helpful to see both sides presented calmly.
Don't be fooled by the mainstream narrative – they're hiding the real truth about these birth control pills and their link to cancer, part of a big pharma agenda to control us all.
Well said, Bret! Let’s keep the discussion fact‑based and respectful. 👍