Introduction to Epigastric Pain and Diverticulitis
As someone who has experienced epigastric pain and learned about diverticulitis, I want to share my knowledge and help others understand the connection between the two. Epigastric pain is a common symptom experienced by many people, and it can have various causes, one of which is diverticulitis. In this article, we will discuss epigastric pain, its causes, symptoms, and treatments, as well as explore the link with diverticulitis.
Understanding Epigastric Pain
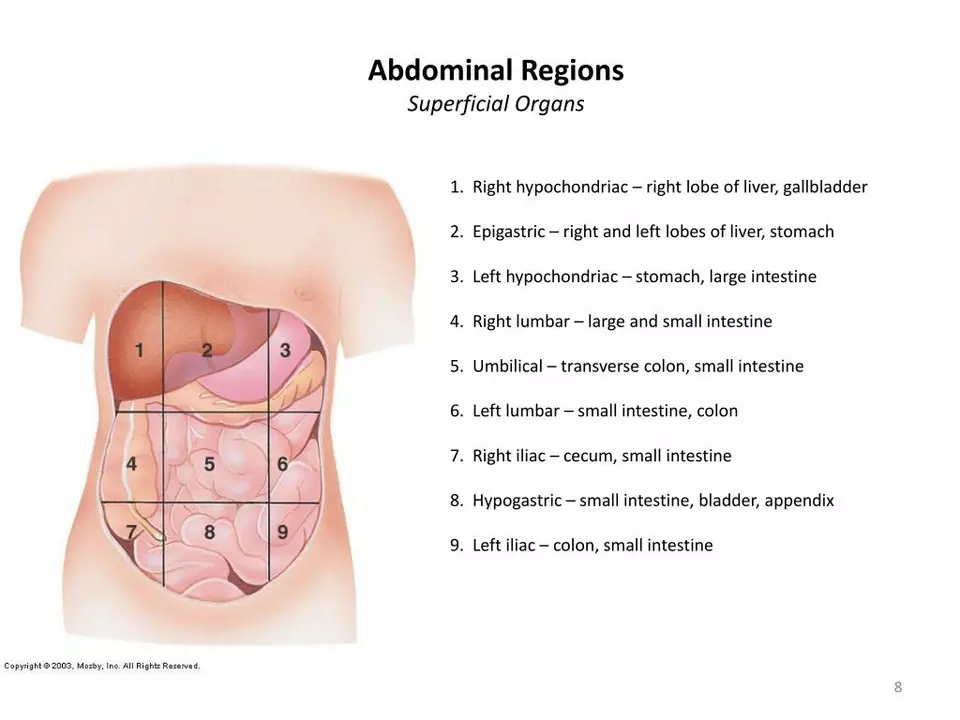
Epigastric pain is a type of discomfort or pain felt in the upper abdomen, usually located just below the ribcage. It can be experienced as a sharp, stabbing pain or a dull, constant ache. The severity of the pain may vary, and it can sometimes radiate to the back or chest. There are several possible causes of epigastric pain, ranging from mild to severe, and it is essential to identify the underlying cause to receive appropriate treatment.
Common Causes of Epigastric Pain
There are numerous potential causes of epigastric pain, some of which include:
- Gastroesophageal reflux disease (GERD)
- Indigestion or dyspepsia
- Gastritis or inflammation of the stomach lining
- Peptic ulcers
- Gallstones or gallbladder inflammation
- Pancreatitis or inflammation of the pancreas
- Diverticulitis
It is crucial to consult with a healthcare professional if you are experiencing persistent or severe epigastric pain to determine the underlying cause and receive appropriate treatment.
What is Diverticulitis?
Diverticulitis is a digestive condition in which small pouches, called diverticula, form in the walls of the colon and become inflamed or infected. These pouches can cause various symptoms, including abdominal pain, fever, and changes in bowel habits. When left untreated, diverticulitis can lead to complications such as abscesses, perforation of the colon, or even a life-threatening infection called peritonitis.
How Diverticulitis Can Cause Epigastric Pain
Diverticulitis can cause epigastric pain due to the inflammation and infection it creates in the colon. When the diverticula become inflamed, they can press against nearby organs and tissues, including the stomach, causing pain in the upper abdomen. Additionally, diverticulitis can lead to other digestive issues, such as constipation or diarrhea, which can further contribute to epigastric pain.
Diagnosing Diverticulitis and Epigastric Pain
If you are experiencing epigastric pain and suspect that diverticulitis may be the cause, it is essential to consult with a healthcare professional. They will likely perform a physical examination and ask about your medical history, symptoms, and any potential risk factors for diverticulitis, such as age and diet. Diagnostic tests may also be ordered, such as blood tests, imaging studies (e.g., CT scan, ultrasound, or X-rays), or a colonoscopy to visualize the colon and determine the presence of diverticula and inflammation.
Treatment Options for Diverticulitis and Epigastric Pain
The treatment for epigastric pain caused by diverticulitis depends on the severity of the condition and the presence of any complications. In mild cases, your healthcare provider may recommend conservative treatments, such as:
- Antibiotics to treat infection
- Pain relievers to manage pain
- A liquid or low-fiber diet to allow the colon to heal
- Probiotics to promote healthy gut bacteria
In more severe cases or if complications are present, more invasive treatments may be necessary, such as surgery to remove the affected portion of the colon.
Preventing Diverticulitis and Epigastric Pain
While it may not always be possible to prevent diverticulitis and the associated epigastric pain, there are steps you can take to reduce your risk:
- Eat a high-fiber diet, including whole grains, fruits, and vegetables, to promote regular bowel movements and reduce pressure in the colon.
- Stay hydrated by drinking plenty of water to help prevent constipation.
- Exercise regularly to support overall digestive health.
- Manage stress, as it can contribute to digestive issues.
By taking these steps, you can help maintain a healthy digestive system and potentially reduce your risk of developing diverticulitis and epigastric pain.
Conclusion
Understanding the connection between epigastric pain and diverticulitis is essential for those who may be experiencing this type of discomfort. By recognizing the symptoms and risk factors, you can seek appropriate medical care and treatment to address the underlying cause and manage your pain. Additionally, adopting a healthy lifestyle and maintaining good digestive health can help prevent the development of diverticulitis and the associated epigastric pain.


6 Comments
Oh great, another genius who thinks epigastric pain is just “a little tummy ache” – newsflash, it’s not.
Hey everyone, just wanted to add that staying hydrated and eating a fiber‑rich diet can really help keep the colon happy and may prevent diverticulitis flare‑ups.
Also, if you experience persistent upper abdominal pain, it's worth getting a CT scan to rule out complications.
Don’t ignore the symptoms – early treatment with antibiotics can keep things from getting serious.
And remember, managing stress and getting regular exercise are simple lifestyle tweaks that support overall gut health.
Hope this helps anyone dealing with that annoying epigastric discomfort!
Thanks for the solid tips, Iris! I wanted to expand a bit – first of all, the connection between diverticulitis and epigastric pain isn’t always obvious because the colon is lower down, but inflammation can radiate upward and affect nearby structures.
Second, each patient’s microbiome is unique, so probiotic strains that work for one person might not for another; it often takes trial and error to find the right mix.
Third, while a high‑fiber diet is the cornerstone of prevention, you have to increase fiber gradually to avoid bloating and gas, which can actually worsen the pain if you jump straight to 30‑grams a day.
Fourth, hydration is key – aim for at least 2‑3 liters of water daily, especially if you’re on a low‑residue diet during a flare.
Fifth, don’t forget the role of NSAIDs; they can irritate the stomach lining and potentially exacerbate epigastric discomfort, so discuss alternatives with your doctor.
Sixth, low‑dose antibiotics like metronidazole are often used for mild diverticulitis, but you need to complete the full course to prevent recurrence.
Seventh, if you have recurring episodes, a colonoscopy isn’t just for diagnosis – it can also help assess the severity of diverticula and guide surgical decisions.
Eighth, watch out for signs of complications such as fever, increasing pain, or changes in bowel habits; these could indicate an abscess or perforation that needs urgent care.
Ninth, some patients find relief with gentle yoga or stretching exercises that promote abdominal muscle relaxation and improve digestion.
Tenth, stress management techniques like deep breathing, meditation, or even a short walk can lower cortisol levels, which in turn may reduce gut inflammation.
Eleventh, keep a symptom diary – noting food intake, stress levels, and pain patterns can help your clinician pinpoint triggers.
Twelfth, remember that not all epigastric pain is diverticulitis; gallbladder disease, pancreatitis, and GERD are common mimickers, so a comprehensive work‑up is essential.
Thirteenth, if imaging shows a large inflamed diverticulum, minimally invasive surgery such as laparoscopic resection may be considered to prevent future attacks.
Fourteenth, after any surgical intervention, a gradual reintroduction of fiber is recommended to allow the gut to heal properly.
Fifteenth, finally, support groups – both online and in‑person – can provide emotional support and practical tips from folks who’ve lived through similar episodes.
Hope this detailed rundown helps anyone navigating the confusing overlap between epigastric pain and diverticulitis.
Wow Sajeev, that was a ton of info! I totally agree that a symptom diary can be a game‑changer – I started one last month and it helped me spot that my pain spikes after I skip breakfast.
Also, the yoga tip is awesome; I’m gonna try some gentle poses tonight.
Don, while your sarcasm is noted, let’s keep it factual: early recognition of epigastric pain, especially when accompanied by fever or elevated white‑blood cells, warrants immediate medical evaluation; antibiotics, dietary modifications, and possibly imaging are standard protocols; ignoring symptoms can lead to severe complications such as perforation, abscess formation, or generalized peritonitis; therefore, a proactive approach is essential.
Hey Emma! 🙌 Great to see you joining the convo – remember, staying positive and keeping that diary can really boost your confidence 😊. If you ever feel stuck, just hit the gym for a quick 15‑minute cardio session – it’s amazing for gut motility! Keep pushing, you’ve got this! 💪